Psoriatic Arthritis: Navigating the Complex Connection
Introduction
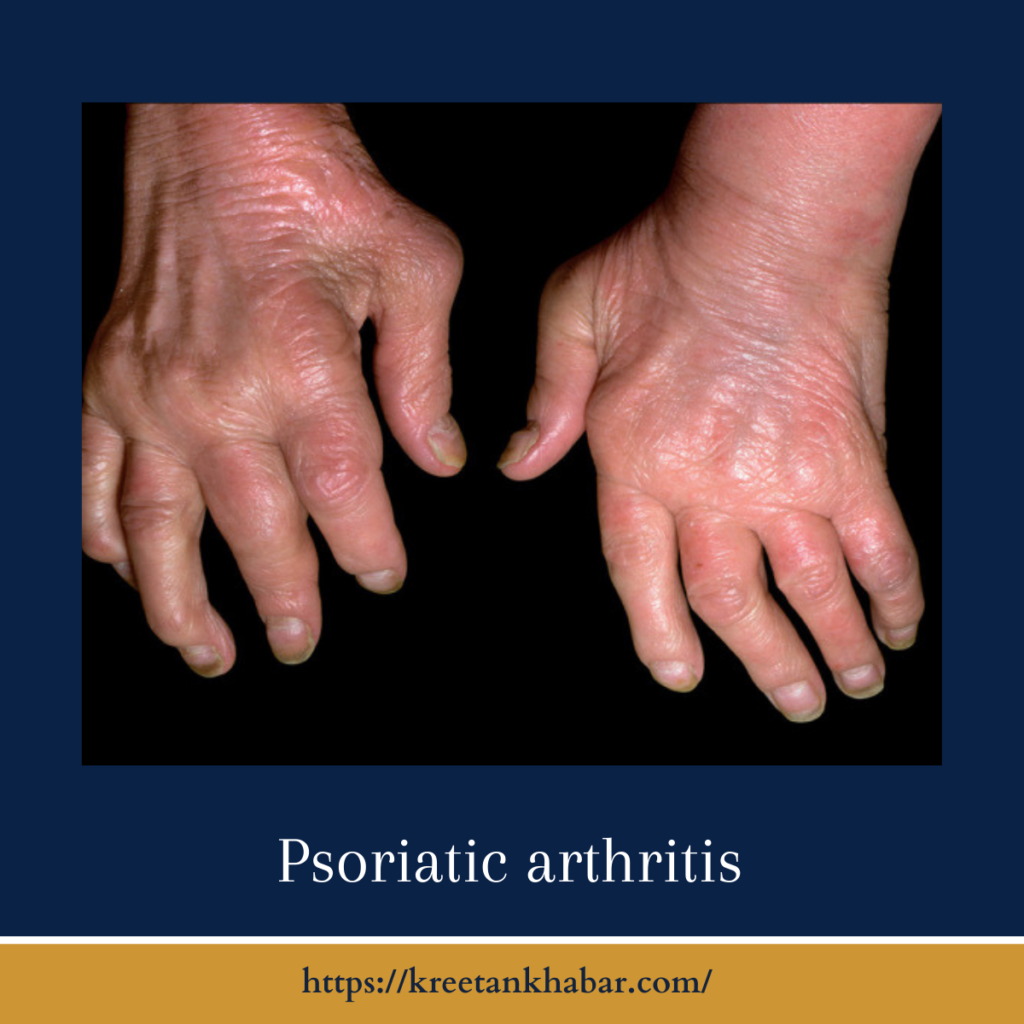
Psoriatic arthritis (PsA) is a multifaceted autoimmune condition that often emerges in individuals with psoriasis, a chronic skin disorder. While it primarily affects the joints, PsA can have widespread systemic effects, making it a challenging and intriguing subject in the realm of rheumatology. In this article, we will delve into the intricate world of psoriatic arthritis, exploring its causes, symptoms, diagnosis, and management.
The Psoriatic Connection
Psoriatic arthritis shares a unique connection with psoriasis, a skin condition characterized by scaly patches of skin. Although not all individuals with psoriasis develop PsA, the two conditions often go hand in hand. PsA can manifest at any age, but it most commonly appears between the ages of 30 and 50. The exact cause of PsA remains unknown, but it is believed to involve a combination of genetic, environmental, and immune system factors.
Symptoms of Psoriatic Arthritis
Psoriatic arthritis is known for its diverse range of symptoms, which can vary from person to person. Common manifestations include:
- Joint Pain and Swelling: PsA primarily affects the joints, leading to pain, stiffness, and swelling. These symptoms can affect any joint, including the fingers, toes, knees, and spine.
- Psoriasis: Many individuals with PsA also have psoriasis, with skin symptoms often appearing before joint symptoms.
- Nail Changes: PsA can cause nail problems such as pitting, ridges, or separation from the nail bed (onycholysis).
- Tenderness: Tenderness or discomfort at the points where tendons and ligaments attach to bones, known as enthesitis, is a common symptom.
- Dactylitis: Also known as “sausage fingers” or “sausage toes,” dactylitis is a distinctive swelling of an entire finger or toe.
- Fatigue: The chronic inflammation associated with PsA can lead to fatigue, which can be quite debilitating.
- Eye Inflammation: Uveitis or inflammation of the eye is a potential complication of PsA, causing eye pain and redness.
here are five unique points about the symptoms of Psoriatic Arthritis (PsA):
- Asymmetrical Joint Involvement: Unlike some other forms of arthritis, Psoriatic Arthritis often affects joints asymmetrically. This means that it can involve joints on one side of the body but not the other, leading to varying degrees of pain and swelling in different joints.
- Enthesitis: Enthesitis, the inflammation of the areas where tendons and ligaments attach to bones, is a hallmark symptom of PsA. This can cause discomfort and tenderness at these attachment points, commonly in the heels, elbows, or the bottom of the feet.
- Nail Changes: PsA can lead to nail abnormalities, such as pitting (small dents or depressions), thickening, or even separation of the nail from the nail bed. These changes in the nails are distinct features often seen in PsA.
- Sausage-Like Fingers or Toes: Dactylitis, also known as “sausage fingers” or “sausage toes,” is a unique symptom of PsA. It results in the swelling of an entire digit, giving it a distinct appearance.
- Silent Spine Involvement: PsA can affect the spine, leading to inflammation and pain in the neck and lower back. Interestingly, some individuals may not experience noticeable symptoms despite having spine involvement, making regular monitoring essential for early detection.
These distinctive symptoms, often occurring alongside skin psoriasis, contribute to the complexity of Psoriatic Arthritis and require a specialized approach to diagnosis and management.
Diagnosis and Management
Diagnosing PsA often requires a thorough evaluation by a rheumatologist. The diagnostic process includes a review of medical history, physical examination, imaging studies (X-rays, MRI), and blood tests to rule out other conditions. Key principles in managing PsA include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologics are commonly prescribed to manage inflammation and slow disease progression.
- Pain Management: Pain relief strategies, such as physical therapy, exercise, and hot/cold therapy, can help alleviate joint discomfort.
- Lifestyle Modifications: Maintaining a healthy lifestyle with regular exercise, a balanced diet, and stress management can help manage PsA symptoms.
- Psoriasis Management: Treating psoriasis effectively can sometimes alleviate PsA symptoms as well.
- Monitoring and Regular Checkups: Frequent follow-ups with healthcare providers are essential to monitor disease activity and adjust treatment as needed.
here are unique insights into the diagnosis and management of Psoriatic Arthritis (PsA):
Diagnosis:
- Medical History and Physical Examination: The diagnosis of Psoriatic Arthritis typically begins with a thorough medical history review and a physical examination. Identifying a history of psoriasis, even if not active at the time, is crucial.
- Imaging Studies: X-rays, MRI scans, and ultrasound imaging can reveal joint and tissue abnormalities associated with PsA. These imaging tests help assess the extent and severity of the disease.
- Blood Tests: While there is no specific blood test for PsA, certain markers like elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may indicate inflammation in the body.
- Nail and Skin Examination: Assessing the nails and skin for psoriasis-related changes, such as pitting or plaques, can provide valuable diagnostic clues.
Management:
- Medications: The choice of medications depends on the severity of PsA. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help relieve pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) like methotrexate are used to slow the progression of the disease. Biologic drugs, such as TNF inhibitors, target specific immune responses and have shown effectiveness in managing PsA.
- Pain Management: Besides medication, various pain management techniques can be beneficial. Physical therapy and exercise programs can improve joint mobility and reduce pain. Heat and cold therapy can offer relief from joint discomfort.
- Lifestyle Modifications: Adopting a healthy lifestyle is essential. Regular exercise, maintaining a balanced diet, and managing stress can contribute to overall well-being and help manage PsA symptoms.
- Psoriasis Management: Treating psoriasis concurrently is often necessary, as it can alleviate PsA symptoms. Topical creams, phototherapy, or systemic medications may be prescribed by dermatologists.
- Regular Monitoring: Close monitoring of PsA is crucial. Regular follow-up appointments with a rheumatologist help track disease activity and make necessary treatment adjustments.
- Joint Protection: Learning joint protection techniques can help individuals with PsA minimize stress on affected joints during daily activities.
- Surgery: In severe cases with joint damage, surgical options like joint replacement or synovectomy (removing inflamed joint lining) may be considered.
- Patient Education: Educating patients about their condition, including its triggers, treatment options, and the importance of medication adherence, empowers them to actively manage their PsA.
- Support Groups: Joining support groups or seeking psychological counseling can help individuals cope with the emotional challenges of living with a chronic condition like PsA.
- Emerging Therapies: Stay informed about emerging treatments and therapies through discussions with healthcare providers and participation in clinical trials when appropriate.
In conclusion, early diagnosis and a multifaceted approach to management are pivotal in effectively addressing Psoriatic Arthritis. By combining medication, lifestyle adjustments, pain management, and regular monitoring, individuals with PsA can lead fulfilling lives while effectively managing their condition.
Conclusion
Psoriatic arthritis is a complex condition that requires a comprehensive and personalized approach to diagnosis and management. With early intervention and ongoing care, individuals with PsA can achieve improved quality of life and better control over their symptoms. By unraveling the intricate connection between psoriasis and arthritis, healthcare professionals and patients alike can navigate the challenges of PsA with greater understanding and optimism for the future.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023