Huntington’s Disease: Unraveling the Mystery of a Devastating Inherited Disorder
Introduction
Huntington’s disease, often abbreviated as HD, is a rare and debilitating genetic disorder that profoundly affects an individual’s neurological and physical functions. This hereditary condition is caused by a mutation in a single gene and can have a profound impact on the affected individual as well as their family. In this article, we will delve into the intricacies of Huntington’s disease, exploring its causes, symptoms, diagnosis, treatment options, and the ongoing research efforts aimed at understanding and managing this complex condition.
Understanding Huntington’s Disease
- Genetic Basis: Huntington’s disease is an autosomal dominant genetic disorder, meaning that a single copy of the mutated gene from either parent is sufficient to cause the disease. The gene responsible for HD is called the HTT gene, which produces a protein known as huntingtin.
- Mutation in the HTT Gene: HD is primarily caused by an abnormal expansion of a specific segment of the HTT gene called CAG repeats. Normally, this segment contains fewer repeats, but in individuals with HD, it is significantly expanded, leading to the production of a mutated huntingtin protein.
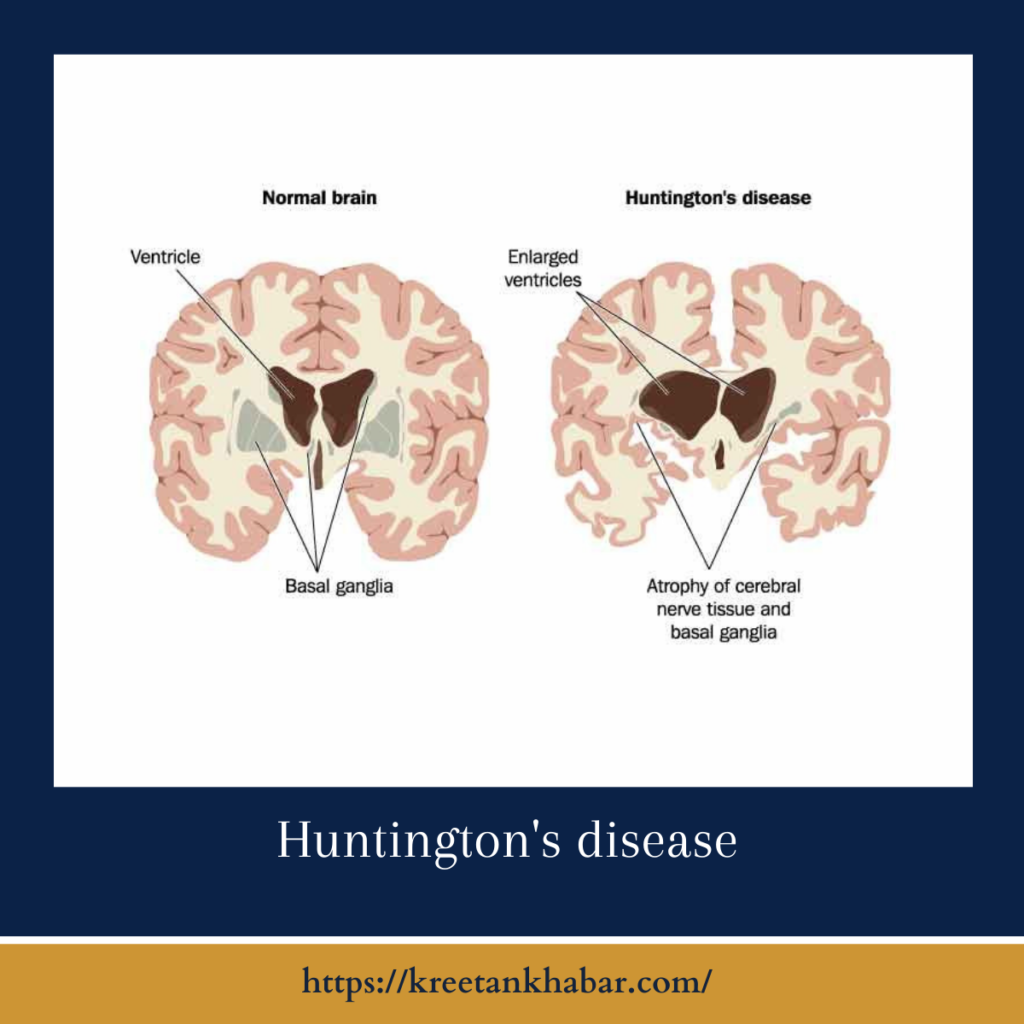
- Neurodegenerative Nature: Huntington’s disease is characterized by progressive degeneration of neurons (nerve cells) in certain regions of the brain, particularly the basal ganglia and cortex. This neuronal loss results in the hallmark symptoms of the disease.
Symptoms and Clinical Manifestations
- Motor Symptoms:
- Involuntary muscle movements, such as chorea (jerky, random movements)
- Rigidity and stiffness
- Difficulty with coordination and balance
- Cognitive Symptoms:
- Impaired thinking and reasoning abilities
- Memory problems
- Difficulty in planning and organizing tasks
- Psychiatric Symptoms:
- Depression
- Anxiety
- Irritability
- Mood swings
- Psychosis (hallucinations and delusions)
- Progressive Nature: Symptoms of HD tend to worsen over time, leading to severe disability and loss of independence.
Diagnosis
- Genetic Testing: The definitive diagnosis of Huntington’s disease is made through genetic testing, which identifies the presence of the mutated HTT gene with expanded CAG repeats.
- Clinical Assessment: Neurologists and genetic counselors conduct comprehensive clinical evaluations to assess motor, cognitive, and psychiatric symptoms. Imaging tests like MRI may also be used to observe brain changes.
Treatment and Management
- Symptomatic Management: While there is no cure for HD, various medications can help manage symptoms, including drugs to reduce chorea and treat mood disorders.
- Physical and Occupational Therapy: These therapies can assist in maintaining mobility, flexibility, and independence for as long as possible.
- Psychological Support: Counseling, psychotherapy, and support groups can help individuals and families cope with the emotional and psychological challenges associated with HD.
- Genetic Counseling: Individuals at risk for HD or those with a family history of the disease may benefit from genetic counseling to make informed decisions about testing and family planning.
here are some key points about the treatment and management of Huntington’s disease:
- Multidisciplinary Approach: The management of Huntington’s disease (HD) typically involves a multidisciplinary team of healthcare professionals, including neurologists, genetic counselors, psychiatrists, physical and occupational therapists, and social workers.
- Symptomatic Treatment:
- Medications: Certain drugs can help manage specific symptoms of HD. For instance, tetrabenazine may reduce chorea (involuntary movements), while antidepressants can address mood disorders.
- Antipsychotic medications may be prescribed to manage psychiatric symptoms like psychosis.
- Physical and Occupational Therapy:
- Physical therapy: Focuses on maintaining mobility, strength, and balance, helping individuals with HD to manage motor symptoms.
- Occupational therapy: Assists in preserving daily living skills and independence.
- Speech and Swallowing Therapy: As HD progresses, individuals may experience difficulty with speech and swallowing. Speech therapy can help address these challenges.
- Psychological Support:
- Counseling and psychotherapy can help individuals and families cope with the emotional and psychological aspects of HD.
- Support groups provide a forum for sharing experiences and receiving mutual support.
- Genetic Counseling:
- Genetic counselors can help individuals at risk for HD make informed decisions about genetic testing, family planning, and options for prenatal testing.
- Nutritional Support: As swallowing difficulties can lead to malnutrition, maintaining a balanced diet and, in some cases, considering a feeding tube may be necessary.
- Medication Management:
- Continual medication management is essential to address changing symptoms and side effects.
- Medications should be adjusted to meet an individual’s evolving needs.
- Clinical Trials: Participation in clinical trials for potential disease-modifying treatments is an option for individuals with HD. These trials aim to slow or halt disease progression.
- Advance Care Planning:
- Individuals with HD and their families should engage in advance care planning discussions.
- Establishing healthcare proxies and documenting preferences for end-of-life care is crucial.
- Research and Hope:
- Ongoing research is focused on understanding the genetic and molecular mechanisms of HD.
- Clinical trials for potential treatments offer hope for future interventions.
- Quality of Life Focus:
- The goal of HD management is to improve the individual’s quality of life by addressing symptoms and providing emotional and social support.
- Patient and Caregiver Education:
- Education about the disease, its progression, and available resources can empower individuals and caregivers to make informed decisions and manage the challenges of HD.
- Regular Follow-Up:
- Regular visits to healthcare providers, including neurologists and other specialists, are essential for monitoring disease progression and adjusting treatment plans.
- Home Modifications: Depending on the individual’s needs, home modifications, such as installing handrails or ramps, may be necessary to enhance safety and accessibility.
- Legal and Financial Planning: Individuals and families should consider legal and financial planning, including estate planning and long-term care arrangements.
Managing Huntington’s disease is a complex and evolving process that requires a personalized approach tailored to the individual’s unique needs and symptoms. Collaboration among healthcare professionals, support from loved ones, and staying informed about the latest advancements in HD research are vital elements in improving the lives of those affected by this challenging condition.
Research and Hope
- Ongoing Research: Scientific research is continually advancing our understanding of HD. Efforts are focused on developing disease-modifying treatments to slow or halt disease progression.
- Clinical Trials: Clinical trials are underway to test potential therapies, offering hope for future treatments that may change the course of the disease.
Conclusion
Huntington’s disease is a complex and devastating condition that affects not only individuals but also their families. While there is no cure for HD, ongoing research holds promise for improved treatments and a better understanding of the disease’s underlying mechanisms. With early diagnosis, symptomatic management, and comprehensive support systems, individuals with HD and their loved ones can navigate the challenges of this genetic disorder with resilience and hope for a brighter future.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023