Crohn’s Disease: A Complex Chronic Condition
Crohn’s disease (also known as ileitis) is a chronic inflammatory bowel disease (IBD) that affects millions of people worldwide. It is a complex condition characterized by inflammation and damage to various parts of the digestive tract. In this article, we’ll delve into the details of Crohn’s disease, including its causes, symptoms, diagnosis, and management.
What is Crohn’s Disease?
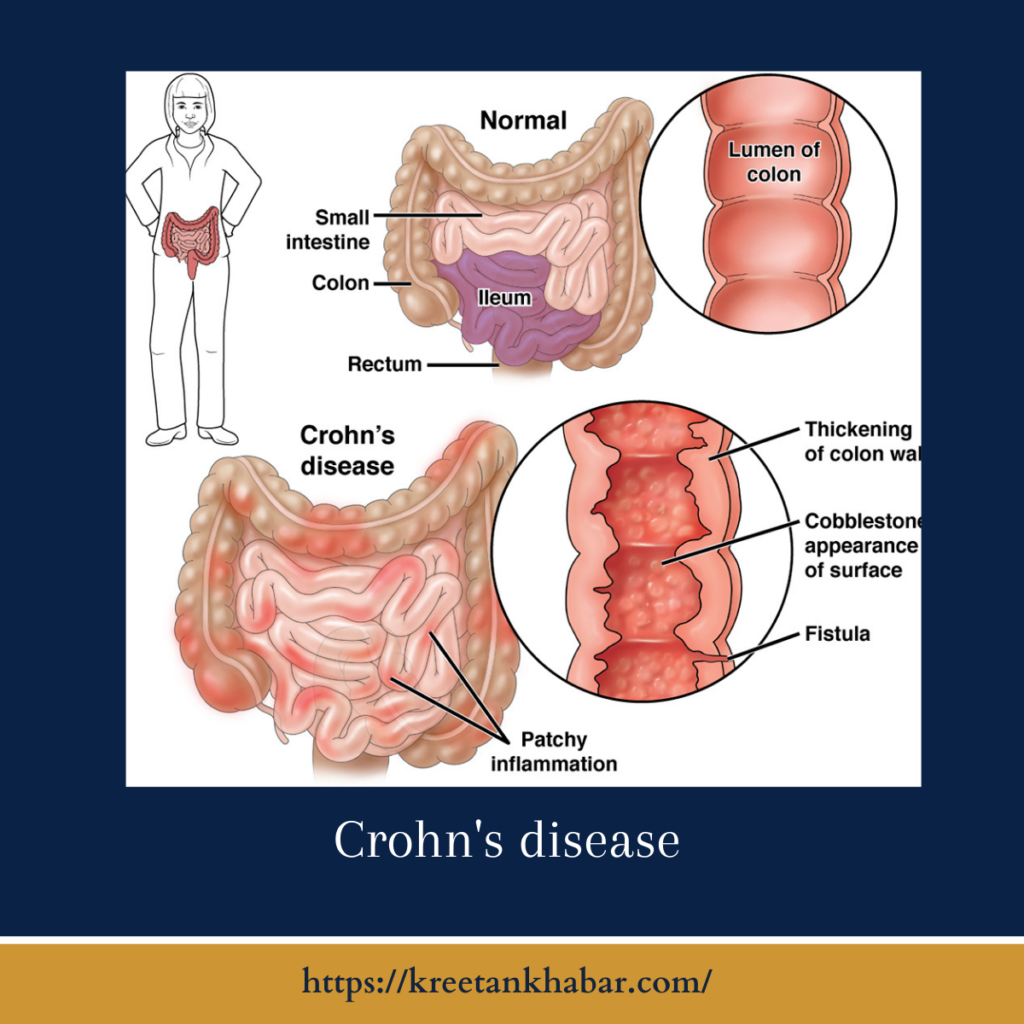
Crohn’s disease is a type of inflammatory bowel disease that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. It is characterized by chronic inflammation, which can lead to a range of symptoms and complications. Crohn’s disease is different from ulcerative colitis, another common form of IBD, which primarily affects the colon and rectum.
Causes of Crohn’s Disease:
The exact cause of Crohn’s disease is still not fully understood, but it is believed to result from a combination of factors, including:
- Genetics: Family history plays a significant role, as individuals with a family member with ileitis are at a higher risk.
- Immune System: Abnormal immune responses may trigger inflammation in the digestive tract.
- Environmental Factors: Certain environmental factors, such as diet, smoking, and exposure to certain infections, may contribute to the development of ileitis.
here are key points describing the possible causes and factors contributing to ileitis:
- Complex Etiology: The exact cause of Crohn’s disease remains unknown, but it is believed to be a multifactorial condition with various contributing elements.
- Genetic Predisposition: Genetics play a significant role in Crohn’s disease. Individuals with a family history of the condition have a higher risk, indicating a genetic predisposition.
- Immune System Dysfunction: An abnormal immune response is thought to be a central factor. In ileitis, the immune system mistakenly attacks the digestive tract, leading to chronic inflammation.
- Environmental Factors: Certain environmental factors may trigger or exacerbate Crohn’s disease. These factors can include:
- Smoking: Smoking is a well-established risk factor for Crohn’s disease, and it can also make the condition more severe.
- Diet: While diet alone does not cause Crohn’s disease, certain dietary factors may influence symptom severity. High intake of processed foods, fats, and sugars and low intake of fruits and vegetables have been associated with the condition.
- Infections: Some researchers suggest that exposure to specific infections, especially in childhood, may increase the risk of developing ileitis.
- Intestinal Microbiota: The gut microbiome, composed of trillions of bacteria, viruses, and fungi, plays a significant role in digestive health. Alterations in the composition of the gut microbiota have been linked to ileitis.
- Autoimmune Component: Crohn’s disease shares some characteristics with autoimmune diseases, where the immune system attacks the body’s tissues. However, it is not classified as a classic autoimmune disease.
- Environmental Triggers: Environmental factors such as stress, diet, and exposure to pollutants may trigger or exacerbate symptoms in individuals with a genetic predisposition.
- Geographical and Ethnic Differences: The prevalence of Crohn’s disease varies geographically, with higher rates observed in developed countries. There are also some ethnic and racial differences in susceptibility.
- Hormonal Factors: Some studies suggest that hormonal factors may play a role, as women are more likely to develop ileitis than men.
- Age and Onset: Crohn’s disease can occur at any age, but it most commonly starts in adolescence or early adulthood.
- Immune System Imbalance: An imbalance in the immune system, involving an overproduction of pro-inflammatory cytokines, contributes to inflammation in the digestive tract.
It’s important to note that while these factors are associated with ileitis, it is a complex condition with individual variability. The interplay between genetics, immune system function, and environmental factors likely contributes to its development. Researchers continue to investigate these factors to gain a better understanding of the disease and improve treatment options.
Symptoms of Crohn’s Disease:
The symptoms of Crohn’s disease can vary widely among individuals and may include:
- Abdominal Pain: Crampy, abdominal pain is a common symptom, often occurring in the lower right side of the abdomen.
- Diarrhea: Persistent, often bloody or mucus-filled diarrhea is a hallmark symptom.
- Weight Loss: Reduced appetite and malabsorption of nutrients can lead to weight loss.
- Fatigue: Chronic inflammation can cause fatigue and reduced energy levels.
- Fever: Some individuals may experience fever as a result of inflammation.
- Rectal Bleeding: Blood in the stool or bleeding from the rectum may occur.
- Loss of Appetite: Reduced appetite and changes in eating habits are common.
- Perianal Symptoms: Inflammation may lead to perianal complications, such as abscesses and fistulas.
Diagnosis of Crohn’s Disease:
Diagnosing ileitis typically involves a combination of the following:
- Medical History: A detailed medical history helps identify symptoms and risk factors.
- Physical Examination: A physical examination may reveal abdominal tenderness or other signs of inflammation.
- Blood Tests: Blood tests can check for markers of inflammation and assess nutritional status.
- Imaging: Imaging tests like CT scans, MRI, or endoscopy (colonoscopy or upper endoscopy) may be used to visualize the GI tract and assess the extent of inflammation.
- Biopsy: During endoscopy, tissue samples (biopsies) may be taken to confirm the diagnosis and rule out other conditions.
Management and Treatment of Crohn’s Disease:
While there is no cure for Crohn’s disease, various treatments can help manage symptoms and control inflammation:
- Medications: Depending on the severity and location of inflammation, medications such as anti-inflammatory drugs, immunosuppressants, and biologics may be prescribed.
- Dietary Changes: Some individuals find relief by making dietary modifications, such as avoiding trigger foods or following a low-residue diet.
- Nutritional Therapy: Nutritional supplements or enteral nutrition may be recommended, especially in cases of malnutrition.
- Lifestyle Modifications: Smoking cessation, stress management, and regular exercise can help manage symptoms.
- Surgery: In severe cases or when complications arise, surgery may be necessary to remove damaged portions of the digestive tract or treat complications like abscesses and fistulas.
- Regular Monitoring: Ongoing monitoring and follow-up with a healthcare provider are essential to adjust treatment as needed and manage the disease effectively.
Conclusion:
Crohn’s disease is a chronic inflammatory bowel disease that requires long-term management. With proper treatment and care, many individuals with ileitis can lead fulfilling lives while effectively managing their symptoms and preventing complications. Early diagnosis and a multidisciplinary approach involving healthcare providers, dietitians, and gastroenterologists are crucial for optimizing the management of this complex condition.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023