Subarachnoid Hemorrhage: A Journey into the Intricate Realms of the Brain
Introduction:
Nestled within the protective layers of the brain, the subarachnoid space is a delicate arena that harbors the cerebral spinal fluid. Yet, amidst this intricate web, a silent intruder may emerge, disrupting the delicate balance—subarachnoid hemorrhage. In this exploration of the mysteries surrounding this condition, we embark on a journey into the profound realms of the brain to understand the causes, symptoms, and the complexities of treatment for subarachnoid hemorrhage.
Understanding Subarachnoid Hemorrhage:
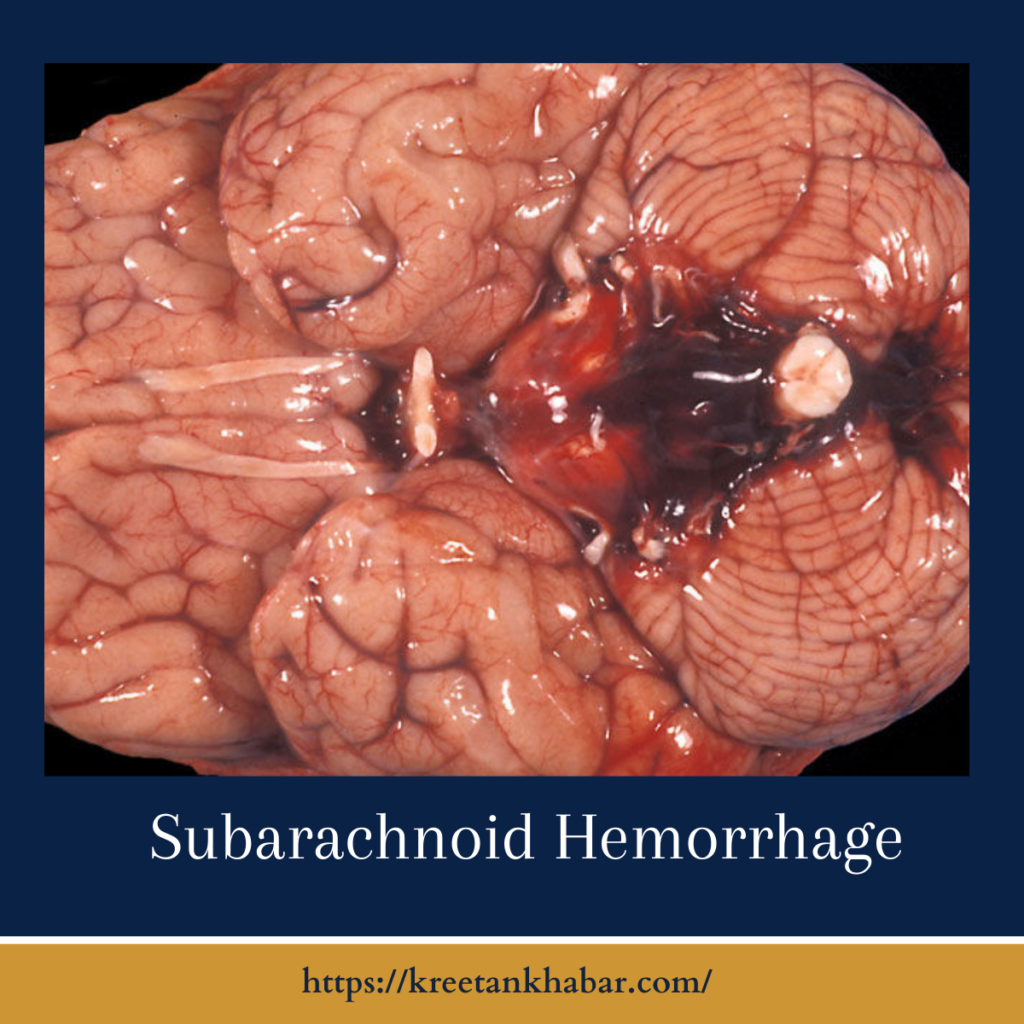
Subarachnoid hemorrhage (SAH) is a neurological emergency characterized by the sudden bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater, two of the three protective layers covering the brain. Typically caused by the rupture of an intracranial aneurysm or less commonly by head trauma, subarachnoid hemorrhage demands immediate attention due to its potential for severe complications.
Causes:
Subarachnoid hemorrhage, akin to a complex symphony of vascular intricacies, can be set into motion by various orchestrators. One primary culprit is the rupture of an intracranial aneurysm, those subtle, balloon-like weaknesses in blood vessel walls that, when breached, unleash a torrent of blood into the subarachnoid space. Arteriovenous malformations, an irregular dance of connections between arteries and veins in the brain.
Also hold the potential to provoke this neurological drama. Beyond the realm of vascular anomalies, traumatic head injuries, with their disruptive impact, can coax blood vessels into a perilous rupture, contributing to subarachnoid hemorrhage. As if choreographed by a hidden hand, factors such as hypertension, age, gender, and genetic predispositions further influence this intricate dance, revealing the multifaceted nature of the causes that underscore the emergence of subarachnoid hemorrhage on the neurological stage.
- Aneurysmal Rupture:
- The most common cause of subarachnoid hemorrhage is the rupture of an intracranial aneurysm. These are bulging, weakened areas in the walls of blood vessels that supply the brain. When an aneurysm bursts, it releases blood into the subarachnoid space.
- Arteriovenous Malformations (AVMs):
- Anomalies in the connections between arteries and veins in the brain, known as arteriovenous malformations, can predispose individuals to subarachnoid hemorrhage. The abnormal vessels may rupture, causing bleeding into the subarachnoid space.
- Head Trauma:
- While less common, severe head trauma can lead to subarachnoid hemorrhage. This may occur in the aftermath of accidents, falls, or other traumatic incidents causing injury to blood vessels within the brain.
Symptoms:
Subarachnoid hemorrhage, with its sudden and intense onset, unfurls a cascade of symptoms that echo the urgency of its presence within the intricate recesses of the brain. The initial harbinger often manifests as a thunderclap headache, a forceful proclamation that this is no ordinary ache. Described as the worst headache of one’s life, it heralds the hemorrhage’s disruptive entry. Accompanying this unwelcome guest, neck stiffness ensues.
A silent protest against movement as if the body instinctively senses the fragility within. Nausea and vomiting join the symphony, a dissonant note in the body’s attempt to cope with the escalating pressure. Light sensitivity, sound aversion, and alterations in consciousness further underscore the severity of the intrusion. It’s a nuanced orchestra of distress, each instrument playing a role in narrating the urgent story of a subarachnoid hemorrhage, demanding swift attention to decipher and alleviate the profound symphony of symptoms it orchestrates.
- Sudden and Severe Headache:
- Often described as the “worst headache of my life,” the sudden onset of an intense headache is a hallmark symptom of subarachnoid hemorrhage.
- Stiff Neck:
- Irritation of the meninges, the membranes covering the brain and spinal cord, can lead to neck stiffness, making it painful to move the head.
- Nausea and Vomiting:
- Increased intracranial pressure can induce nausea and vomiting, which may be persistent and unrelated to dietary factors.
- Photophobia (Light Sensitivity) and Phonophobia (Sound Sensitivity):
- Sensitivity to light and sound can accompany subarachnoid hemorrhage due to the irritation of the meninges.
- Altered Mental Status:
- Confusion, drowsiness, or even loss of consciousness can occur as a result of the bleeding affecting normal brain function.
- Seizures:
- In some cases, subarachnoid hemorrhage may provoke seizures, further complicating the clinical picture.
Treatment:
Navigating the aftermath of a subarachnoid hemorrhage demands a delicate balance of medical interventions, resembling a meticulous tapestry woven to restore stability to the intricate landscape of the brain. Immediate and decisive action is paramount, often beginning with emergency measures to stabilize the patient and alleviate the surge in intracranial pressure. Diagnosis through imaging techniques, such as CT scans and lumbar punctures, guides the subsequent steps. For cases arising from the rupture of an intracranial aneurysm, neurosurgical prowess comes to the fore.
Aneurysm clipping or coiling, intricate procedures designed to seal the breach and prevent further bleeding, are deployed with surgical precision. Concurrently, meticulous blood pressure management becomes a therapeutic thread, crucial in averting the peril of rebleeding. Pain management and supportive measures, including medications to alleviate discomfort and control nausea, are woven seamlessly into the treatment tapestry. As the patient embarks on the path of recovery, the collaborative efforts of medical professionals, akin to skilled artisans, continue to shape the narrative, striving to mend the delicate fabric of the brain and restore hope to those affected by the complex aftermath of subarachnoid hemorrhage.
- Emergency Medical Attention:
- Subarachnoid hemorrhage is a medical emergency that requires immediate attention. Emergency medical services should be contacted promptly to ensure timely transport to the hospital.
- Diagnostic Imaging:
- CT scans and lumbar punctures are common diagnostic tools used to confirm the presence of subarachnoid hemorrhage and identify its underlying cause.
- Aneurysm Clipping or Coiling:
- In cases where an aneurysm is identified as the cause, neurosurgical procedures such as clipping or coiling may be performed to prevent further bleeding.
- Blood Pressure Management:
- Blood pressure control is crucial to manage the risk of rebleeding. Medications may be administered to regulate blood pressure levels.
- Pain Management:
- Medications to alleviate pain and discomfort, often including analgesics and antiemetics, may be prescribed.
Conclusion:
Subarachnoid hemorrhage, with its sudden and often dramatic onset, thrusts us into the intricate realms of the brain’s protective layers. Understanding the causes, recognizing the symptoms, and ensuring swift and appropriate medical intervention are paramount in navigating the complexities of subarachnoid hemorrhage. As we unravel the mysteries surrounding this condition, we pave the way for improved awareness, diagnosis, and treatment, offering hope in the face of this formidable neurological challenge.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023