Abdominal Aortic Aneurysm: A Silent Threat
Introduction
Within the intricate network of arteries that supply blood throughout our bodies, the abdominal aorta stands as one of the most critical. However, when this major blood vessel becomes weakened and dilates abnormally, it poses a significant health risk. In this article, we will explore the insidious condition known as abdominal aortic aneurysm (AAA), shedding light on its causes, symptoms, risk factors, diagnosis, and treatment options.
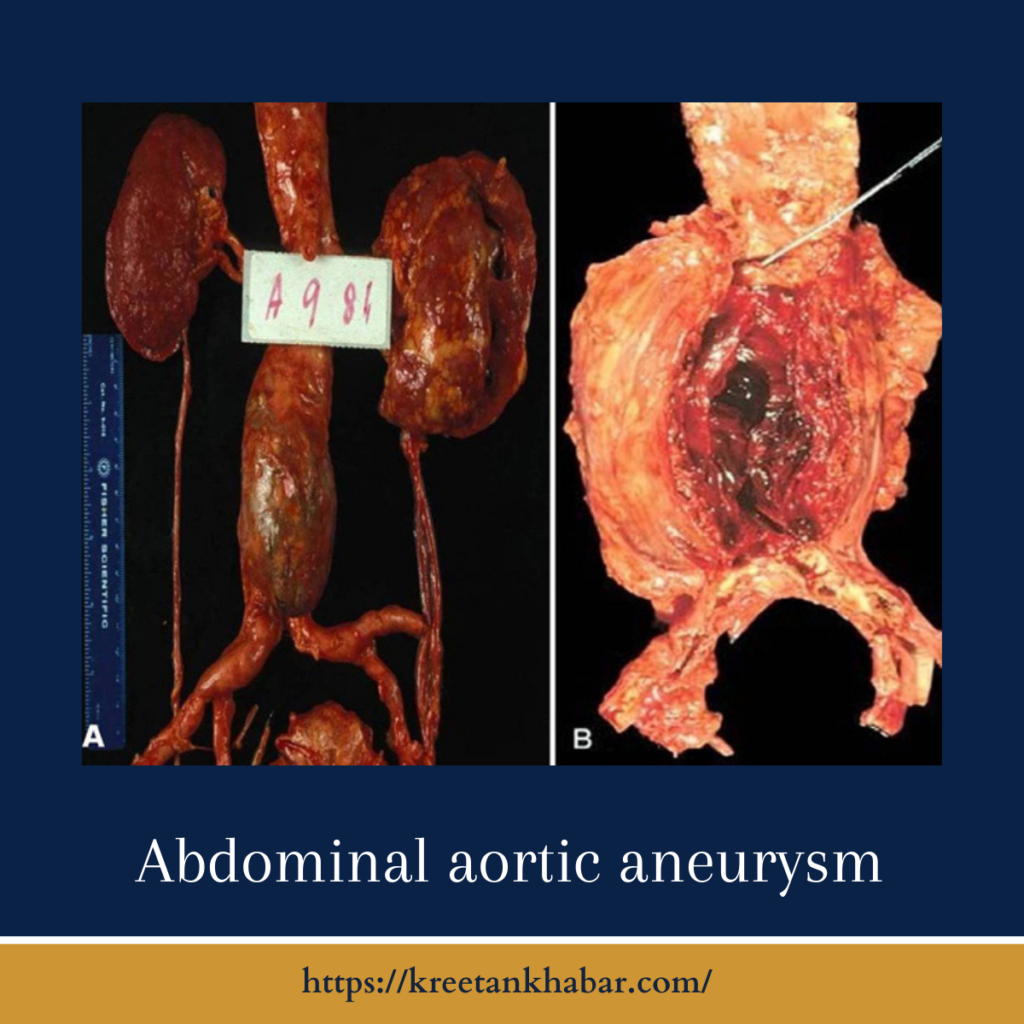
Understanding Abdominal Aortic Aneurysm (AAA)
An abdominal aortic aneurysm is a localized dilation or ballooning of the abdominal aorta, the large blood vessel that carries oxygenated blood from the heart to the lower body. AAA is often referred to as a “silent killer” because it typically develops without noticeable symptoms until it reaches a critical size or ruptures, which can be life-threatening.
Causes of Abdominal Aortic Aneurysm
The exact cause of AAA is multifactorial, but a few key factors contribute to its development:
- Atherosclerosis: The most common underlying cause is the buildup of fatty deposits and cholesterol (atherosclerosis) in the arterial wall.
- High Blood Pressure (Hypertension): Chronic high blood pressure can weaken the arterial wall, making it more susceptible to dilation.
- Genetics: A family history of abdominal aortic aneurysm increases the risk, suggesting a genetic predisposition.
- Age: Advancing age is a significant risk factor, with AAA occurring more frequently in individuals over 65.
- Gender: Men are more likely to develop AAA than women.
- Tobacco Use: Smoking is a major risk factor, as it accelerates atherosclerosis and weakens arterial walls.
- Inflammatory Diseases: Certain conditions, such as vasculitis, can cause inflammation of blood vessels, potentially leading to AAA.
Symptoms of Abdominal Aortic Aneurysm
AAA typically does not present noticeable symptoms until it reaches a critical size or ruptures. When symptoms do occur, they may include:
- Abdominal Pain: Dull, constant pain in the abdomen or back, which may be severe if the aneurysm is about to rupture.
- Pulsating Mass: Some individuals can feel a pulsating mass in the abdomen.
- Limb Discoloration and Pain: In rare cases, if an aneurysm compresses nearby nerves or blood vessels, it can cause leg pain or limb discoloration.
It’s essential to note that many AAAs are discovered incidentally during routine medical examinations or imaging studies for unrelated conditions.
Risk Factors for Abdominal Aortic Aneurysm
Several risk factors increase the likelihood of developing abdominal aortic aneurysm:
- Age: The risk of AAA increases with age, particularly after the age of 65.
- Gender: Men are four to five times more likely to develop abdominal aortic aneurysm than women.
- Smoking: Tobacco use is a significant modifiable risk factor.
- Family History: Having a first-degree relative with AAA elevates the risk.
- Atherosclerosis: Individuals with a history of atherosclerosis are at higher risk.
- High Blood Pressure: Uncontrolled hypertension can weaken the arterial wall.
- Connective Tissue Disorders: Certain genetic conditions, like Marfan syndrome or Ehlers-Danlos syndrome, increase susceptibility.
Diagnosis of Abdominal Aortic Aneurysm
Early diagnosis of AAA is crucial for preventing rupture and managing the condition effectively. Diagnosis methods include:
- Physical Examination: A healthcare provider may detect a pulsating mass during a routine physical exam.
- Imaging: Ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) can confirm the presence and size of an AAA.
- Screening Programs: Some countries offer AAA screening programs, especially for individuals at high risk, such as older men who have ever smoked.
Here are 30 unique points outlining the diagnosis of Abdominal Aortic Aneurysm (AAA):
- Physical Examination: A healthcare provider may detect an AAA during a routine physical examination by feeling a pulsating mass in the abdomen.
- Medical History: Information about family history of AAA, smoking habits, and other risk factors is essential in diagnosing and assessing the risk of AAA.
- Ultrasound: Ultrasonography is a common and non-invasive imaging technique used to visualize the abdominal aorta and confirm the presence of an AAA.
- Abdominal X-ray: A plain abdominal X-ray may reveal a calcified AAA, although it is less commonly used for diagnosis than other imaging methods.
- CT Scan: Computed tomography (CT) scans provide detailed images of the abdominal aorta, allowing precise measurement of the aneurysm’s size and shape.
- MRI: Magnetic resonance imaging (MRI) can offer high-resolution images and is sometimes used for AAA diagnosis.
- Color Doppler Ultrasound: This specialized ultrasound technique helps assess blood flow within the AAA, which can be useful in determining the risk of rupture.
- Contrast-Enhanced CT: A CT scan with contrast dye can provide enhanced visualization of the AAA and its surrounding structures.
- Screening Programs: In some regions, targeted AAA screening programs are available for high-risk populations, such as older men with a history of smoking.
- Aortic Angiography: A more invasive procedure, aortic angiography, involves injecting contrast dye into the aorta and taking X-ray images to visualize the aneurysm.
- CT Angiography: This CT-based angiography provides a detailed view of the blood vessels and is often used to assess the anatomy of the AAA.
- Magnetic Resonance Angiography (MRA): MRA uses magnetic fields and radio waves to create detailed images of blood vessels, including the abdominal aorta.
- Duplex Ultrasound: Duplex ultrasound combines traditional ultrasound with Doppler ultrasound to assess blood flow and the size of the AAA.
- Serial Imaging: For small AAAs, serial imaging through repeated ultrasounds or CT scans may be used to monitor any changes in size over time.
- Risk Assessment: Risk calculators and guidelines are used to determine an individual’s risk of developing an AAA, often based on age, gender, and smoking history.
- Physical Measurements: The diameter of the AAA is measured to determine its size, which plays a crucial role in deciding on treatment options.
- Routine Check-Ups: Regular check-ups with a healthcare provider can aid in the early detection of AAA, especially in individuals with risk factors.
- Emergency Imaging: In cases of suspected AAA rupture, emergency imaging like CT or ultrasound is performed to confirm the diagnosis and assess the severity of bleeding.
- Emergency Surgery: If a ruptured AAA is suspected, emergency surgery is often initiated without extensive imaging to prevent fatal hemorrhage.
- Anatomical Assessment: Imaging helps determine the location of the AAA, whether it is above or below the renal arteries.
- Patient Symptom Evaluation: Symptoms such as abdominal or back pain may prompt immediate imaging to rule out a ruptured AAA.
- Hemodynamic Assessment: Evaluation of blood pressure, heart rate, and other vital signs can provide crucial information about the stability of the AAA.
- Specialized Imaging Centers: Dedicated vascular centers and radiology facilities often provide advanced imaging for AAA diagnosis and management.
- Radiation Exposure Considerations: The choice of imaging method may be influenced by the patient’s radiation exposure history.
- Contrast Allergies: In patients with known contrast allergies, alternative imaging methods may be chosen.
- Patient Comfort: Patient comfort and compliance with imaging procedures are important considerations during AAA diagnosis.
- Follow-Up Imaging: After AAA diagnosis, regular follow-up imaging helps monitor its progression and determine the need for intervention.
- Evaluation of Blood Vessels: In addition to the AAA itself, imaging helps assess the condition of the surrounding blood vessels and branches.
- Surgical Planning: Detailed imaging is essential for surgical planning, enabling the surgeon to select the appropriate technique and graft size.
- Patient Education: Patients diagnosed with AAA should receive education about their condition, treatment options, and the importance of lifestyle modifications
Treatment Options for Abdominal Aortic Aneurysm
The management of AAA depends on its size, location, and the individual’s overall health. Treatment options include:
- Watchful Waiting: Small AAAs (less than 5.5 cm in diameter) are often monitored regularly to track any changes.
- Medications: Blood pressure-lowering medications may be prescribed to reduce the risk of AAA growth.
- Endovascular Repair: Minimally invasive procedures, such as endovascular repair (EVAR) or endovascular aneurysm repair (EVAR), involve the placement of a stent graft to reinforce the weakened arterial wall.
- Open Surgical Repair: Traditional open surgery to remove the aneurysm and replace it with a synthetic graft may be necessary for larger or rapidly growing AAAs.
- Lifestyle Changes: Quitting smoking, managing blood pressure, and adopting a heart-healthy lifestyle are critical for preventing AAA progression.
Conclusion
Abdominal aortic aneurysm is a potentially life-threatening condition that often develops without symptoms until it becomes critical or ruptures. Early
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023