Amyotrophic Lateral Sclerosis (ALS): Understanding the Disease and Embracing Hope
Introduction:
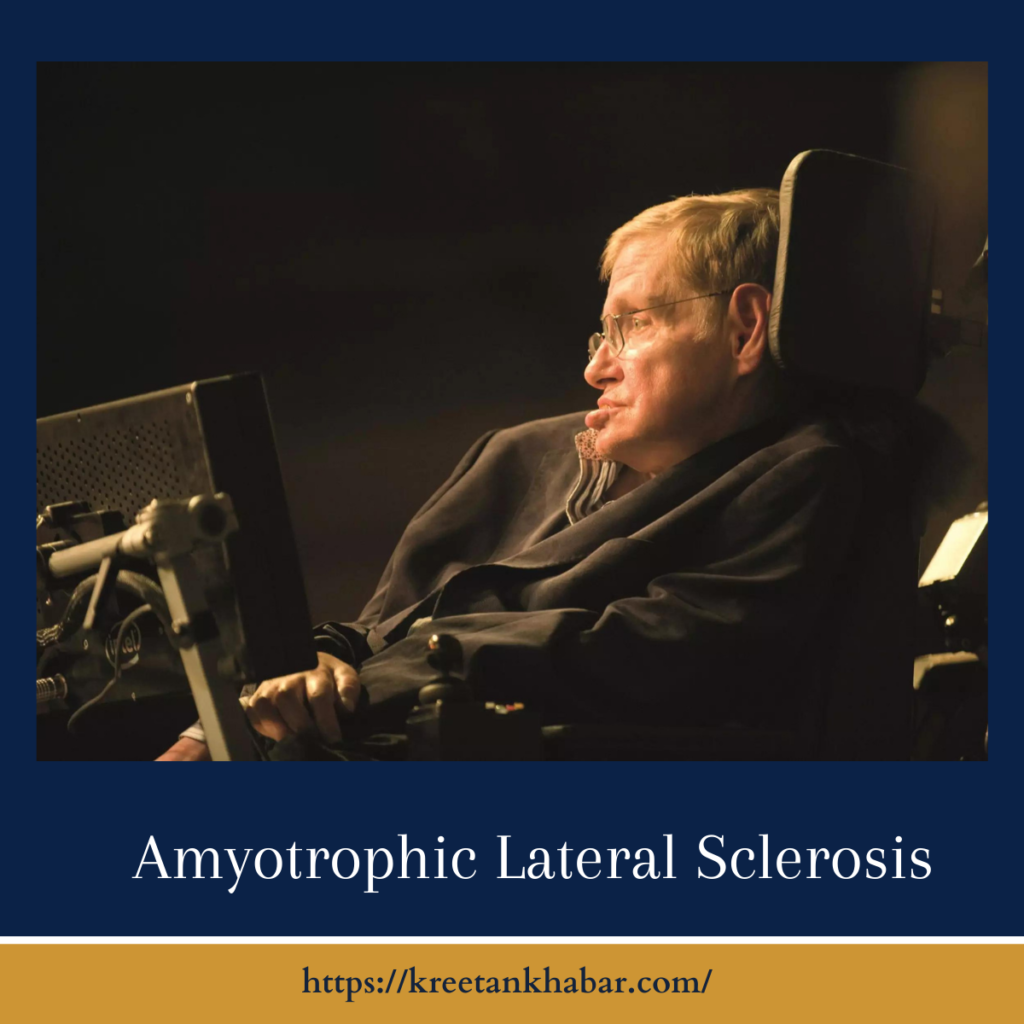
Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig’s disease, is a progressive and devastating neurodegenerative disorder that affects nerve cells in the brain and spinal cord. In this article, we explore the intricacies of Amyotrophic Lateral Sclerosis, its impact on individuals and families, as well as the ongoing efforts to understand and manage this complex condition.
Understanding Amyotrophic Lateral Sclerosis:
ALS is characterized by the gradual degeneration and death of motor neurons, the nerve cells responsible for controlling voluntary muscles. As these motor neurons cease to function, muscles weaken and waste away, eventually leading to paralysis. Amyotrophic Lateral Sclerosis is relentless in its progression, affecting various aspects of motor function, including walking, speaking, swallowing, and breathing.
Causes and Risk Factors:
- Genetic Factors: While most cases of Amyotrophic Lateral Sclerosis are sporadic, approximately 5-10% have a familial component. Specific genetic mutations, such as those in the C9orf72 or SOD1 genes, are associated with an increased risk of familial Amyotrophic Lateral Sclerosis.
- Age: ALS can affect individuals of any age, but it most commonly emerges in people between the ages of 40 and 70, with the risk increasing with age.
- Gender: Men are slightly more likely to develop Amyotrophic Lateral Sclerosis than women, although the reasons for this gender discrepancy are not yet fully understood.
- Environmental Factors: While the majority of Amyotrophic Lateral Sclerosis cases are not directly linked to environmental factors, some studies suggest that exposure to certain toxins or substances may contribute to the risk of developing ALS.
More points of causes and risk factors:
Signs and Symptoms:
- Muscle Weakness: Gradual onset of muscle weakness, typically beginning in the hands or feet, is a hallmark symptom of ALS.
- Difficulty with Fine Motor Skills: Individuals may experience challenges with tasks requiring precision and coordination, such as buttoning a shirt or writing.
- Muscle Cramps and Twitching: Persistent muscle cramps and twitching, known as fasciculations, may occur in affected areas.
- Impaired Speech and Swallowing: ALS can lead to difficulties in speaking and swallowing as the muscles involved in these functions weaken.
- Progressive Paralysis: Over time, ALS progresses to affect larger muscle groups, leading to increasing difficulty in mobility and eventually causing paralysis.
- Respiratory Distress: As the muscles responsible for breathing are affected, individuals with ALS may experience respiratory difficulties, necessitating respiratory support in advanced stages.
Diagnosis:
Diagnosing ALS is a complex process that involves ruling out other conditions with similar symptoms. Key diagnostic steps include a thorough medical history, neurological examinations, electromyography (EMG) to assess muscle function, and imaging studies such as magnetic resonance imaging (MRI).
Management and Treatment:
- Riluzole: The FDA-approved medication riluzole may slow the progression of ALS by reducing the release of glutamate, a neurotransmitter that contributes to nerve cell damage.
- Edaravone: Another FDA-approved drug, edaravone, is believed to have antioxidant effects and is used to manage symptoms in certain cases.
- Supportive Therapies: Physical therapy, occupational therapy, and speech therapy can help individuals maintain functionality and improve their quality of life.
- Assistive Devices: Wheelchairs, communication devices, and other assistive technologies can enhance independence for those with ALS.
Hope Through Research:
Ongoing research aims to unravel the complexities of ALS, seeking a deeper understanding of its mechanisms and potential treatment avenues. Clinical trials and collaborative efforts within the scientific community offer hope for advancements in managing and ultimately finding a cure for this challenging disease.
Conclusion:
Amyotrophic Lateral Sclerosis is a formidable adversary, affecting not only the individuals diagnosed but also their families and caregivers. Despite the profound challenges it poses, ongoing research, supportive care, and the resilience of those impacted by ALS contribute to a collective journey toward understanding, managing, and one day conquering this complex neurodegenerative disorder.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023