Anal Fissure: Causes, Symptoms, Treatment, and Prevention
Introduction
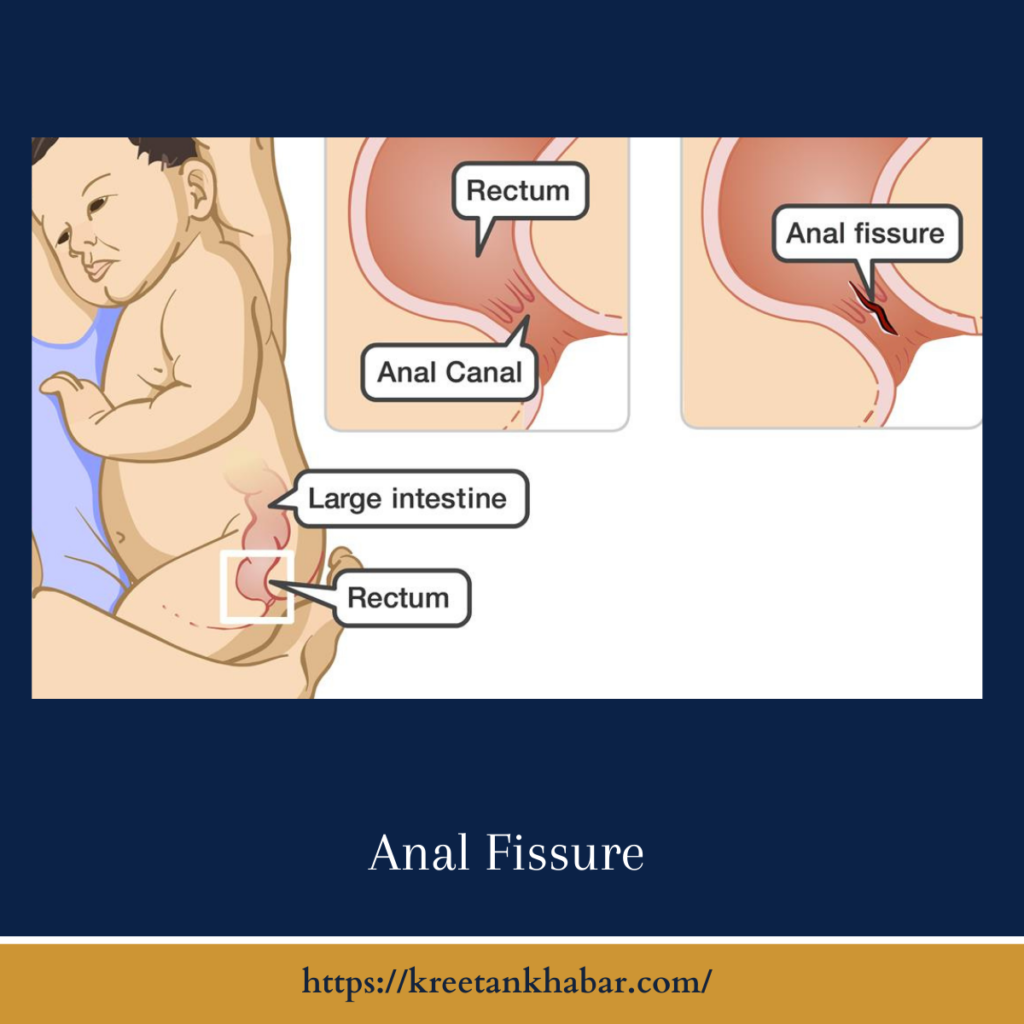
Anal fissures, though often considered a taboo topic, are a common and painful condition affecting many individuals. An anal fissure is a small tear or cut in the lining of the anus, causing discomfort, pain, and even bleeding during bowel movements. In this article, we will delve into the causes, symptoms, treatment options, and prevention strategies for anal fissures.
Causes
- Straining during Bowel Movements: One of the most common causes of anal fissures is excessive straining while passing stool, which can lead to tears in the delicate anal tissue.
- Hard or Large Stools: Constipation, diarrhea, or the passage of hard or large stools can irritate the anal canal and contribute to the development of fissures.
- Chronic Digestive Conditions: Conditions such as Crohn’s disease, ulcerative colitis, and irritable bowel syndrome (IBS) can increase the risk of anal fissures due to frequent bowel movements or inflammation.
- Childbirth: In women, anal fissures can occur during childbirth, particularly in cases of prolonged or difficult labor.
- Anal Trauma: Accidental injuries, including anal sex or the insertion of foreign objects, can cause fissures in the anal lining.
Certainly, here are some common causes of anal fissures explained in a human-like writing style:
- Straining During Bowel Movements: One of the primary causes of anal fissures is excessive straining during bowel movements. When you push too hard to pass stool, the delicate lining of the anus can tear, leading to a fissure.
- Constipation: Chronic constipation is another major factor. When you’re constipated, your stools tend to be hard and difficult to pass. This can put immense pressure on the anal canal, making it more susceptible to fissures.
- Diarrhea: While constipation can cause fissures, the opposite extreme, frequent diarrhea, can also be a culprit. The constant irritation and abrasiveness of loose stools can damage the sensitive anal tissues.
- Large Stool Size: Passing large or hard stools regularly can stretch the anus, making it prone to tearing. This is often seen in people with a low-fiber diet.
- Anal Trauma: Trauma to the anal area, such as from anal intercourse, childbirth, or the insertion of foreign objects, can cause fissures to develop.
- Anal Spasms: In some cases, involuntary anal muscle spasms can make the fissure worse by preventing it from healing properly. These spasms can be caused by various factors, including stress and anxiety.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis, which are types of IBD, can cause chronic inflammation in the digestive tract. This inflammation can extend to the anal area and contribute to fissure formation.
- Age: Anal fissures are more common in young adults and older individuals. In the elderly, the skin in the anal area becomes thinner and less elastic, making it more susceptible to fissures.
- Obesity: Excess body weight can put increased pressure on the abdomen and pelvis, which can lead to the development of fissures, especially if combined with a sedentary lifestyle.
- Poor Hygiene: Inadequate anal hygiene, such as not cleaning the area properly after bowel movements, can increase the risk of anal fissures due to the presence of irritating fecal residue.
- Inadequate Fiber Intake: A diet lacking in fiber can lead to hard stools and constipation, which, as mentioned earlier, are significant factors in fissure development.
- Dehydration: Not drinking enough water can result in harder stools, further contributing to the risk of anal fissures.
It’s important to note that many of these causes are interrelated, and multiple factors may contribute to the development of anal fissures. If someone is experiencing symptoms of an anal fissure, it’s advisable to seek medical attention for proper diagnosis and treatment.
Symptoms
- Pain During Bowel Movements: The most common symptom of anal fissures is severe pain or burning during and after passing stool.
- Bright Red Blood: Fissures often lead to the presence of bright red blood on toilet paper or in the toilet bowl.
- Itching and Discomfort: Individuals with anal fissures may experience persistent itching and discomfort around the anus.
- Muscle Spasms: Some people may also encounter muscle spasms in the anal region, making the condition even more painful.
Treatment
- Dietary Changes: Increasing dietary fiber intake and staying well-hydrated can help soften the stool, making it easier to pass and reducing the risk of further irritation.
- Topical Medications: Over-the-counter or prescription ointments containing nitroglycerin or calcium channel blockers can help relax the anal sphincter muscle and promote healing.
- Sitz Baths: Soaking in warm water, known as a sitz bath, for about 15 minutes a few times a day can provide relief and promote healing.
- Pain Medication: Over-the-counter pain relievers, such as ibuprofen, can help manage the discomfort associated with anal fissures.
- Botox Injections: In some cases, a healthcare provider may recommend Botox injections to relax the anal sphincter and promote healing.
- Surgery: When conservative treatments are ineffective, a surgical procedure known as a lateral internal sphincterotomy may be performed to relax the anal sphincter muscle.
Prevention
- Maintain a High-Fiber Diet: A diet rich in fruits, vegetables, and whole grains can help soften the stool and prevent constipation.
- Stay Hydrated: Drinking an adequate amount of water is crucial for softening the stool and maintaining overall digestive health.
- Avoid Straining: Practice gentle and unhurried bowel movements, and avoid excessive straining.
- Personal Hygiene: Keep the anal area clean and dry, and consider using moist towelettes instead of rough toilet paper.
- Manage Underlying Conditions: If you have an underlying digestive condition, work with your healthcare provider to manage it effectively.
Certainly, here’s a list of practical tips for preventing anal fissures, presented in a human-like writing style:
- Dietary Fiber: Incorporate a diet rich in dietary fiber, including fruits, vegetables, whole grains, and legumes. Fiber helps soften stools and makes them easier to pass, reducing the risk of fissures.
- Hydration: Stay well-hydrated by drinking an adequate amount of water throughout the day. Proper hydration helps maintain soft and regular bowel movements.
- Regular Bowel Habits: Establish a regular bowel routine by visiting the toilet when you feel the urge. Avoid holding in stools, as this can lead to constipation and straining.
- Fiber Supplements: If it’s challenging to get enough fiber through your diet, consider using fiber supplements, as recommended by a healthcare professional.
- Avoid Straining: Make an effort to avoid straining during bowel movements. Relax and allow stools to pass naturally.
- Toilet Training: Teach children proper toilet training techniques to prevent constipation and straining.
- Good Anal Hygiene: After bowel movements, clean the anal area gently but thoroughly using soft, unscented toilet paper or moist towelettes. Avoid excessive scrubbing.
- Warm Water Baths: Soaking in a warm bath (known as a sitz bath) for 15-20 minutes can help relax the anal muscles and promote healing.
- Lubricants: Use a water-based lubricant for anal intercourse to reduce friction and the risk of trauma.
- Regular Exercise: Engage in regular physical activity to help maintain overall digestive health and prevent obesity, which can contribute to anal fissures.
- Manage Stress: Practice stress-reduction techniques like deep breathing, meditation, or yoga, as stress can lead to anal muscle tension and spasms.
- Avoid Harsh Soaps: Choose mild, fragrance-free soaps for anal cleansing to avoid irritating the sensitive anal area.
- Medical Conditions: If you have inflammatory bowel disease (IBD), diabetes, or other medical conditions that increase the risk of anal fissures, work closely with your healthcare provider to manage your condition effectively.
- Medication Review: If you’re taking medications that cause constipation or diarrhea as side effects, discuss potential alternatives or additional treatments with your healthcare provider.
- Maintain Ideal Body Weight: Maintain a healthy body weight through a balanced diet and regular exercise to reduce the strain on your abdominal and anal muscles.
- Consult a Healthcare Provider: If you experience recurring or severe anal fissures, seek medical advice promptly. Your healthcare provider can recommend specialized treatments or surgical options if necessary.
By incorporating these preventive measures into your daily routine, you can significantly reduce the risk of developing anal fissures and maintain better anal health. Remember that prevention is key to avoiding the discomfort and pain associated with this condition.
Conclusion
Anal fissures can be painful and distressing, but they are a common condition that can be managed and treated. By understanding the causes, recognizing the symptoms, seeking appropriate treatment, and following prevention strategies, individuals can alleviate discomfort and promote healing. If you experience persistent anal fissure symptoms, it’s important to consult a healthcare professional for proper diagnosis and guidance.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023