Bowel Incontinence: Understanding, Causes, and Coping Strategies
Introduction
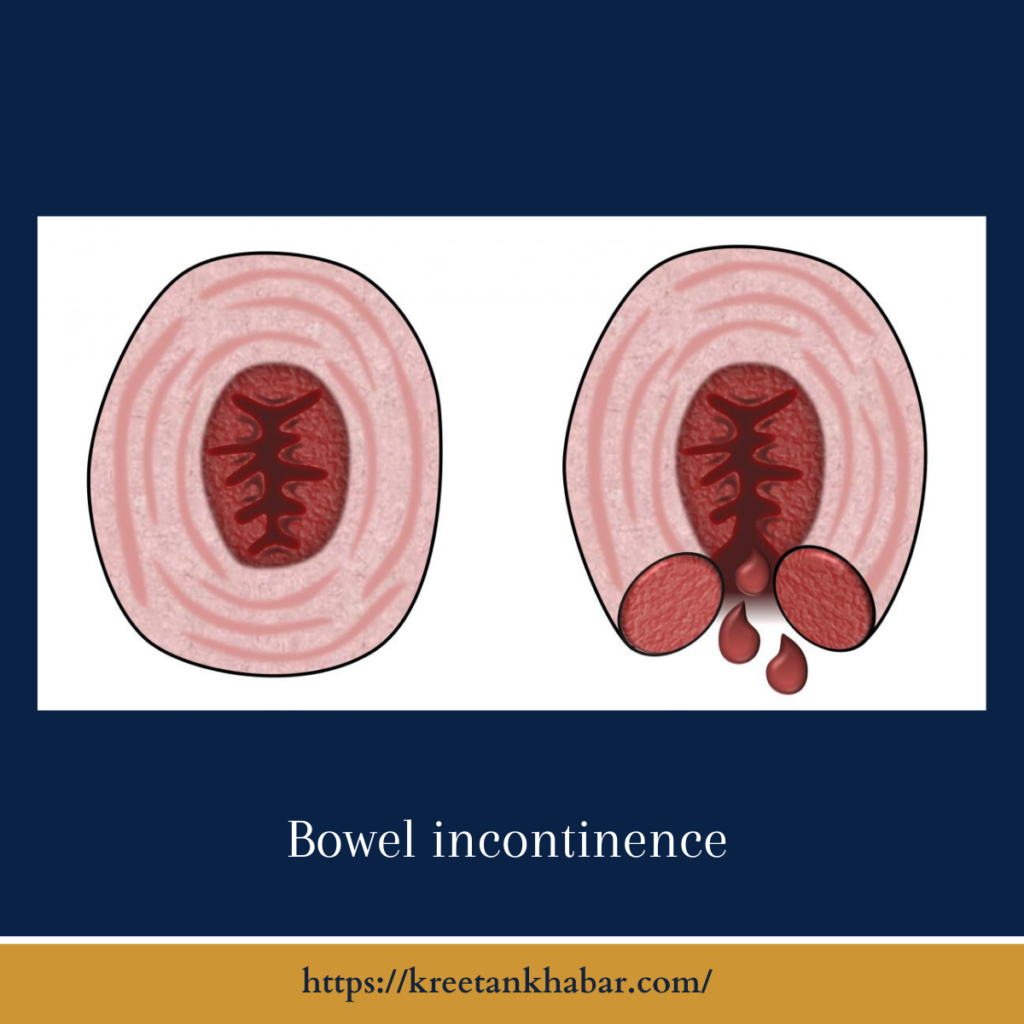
Bowel incontinence, often referred to as fecal incontinence, is a challenging medical condition that can significantly impact an individual’s quality of life. It is characterized by the inability to control bowel movements, leading to involuntary leakage of stool. This condition can be embarrassing and emotionally distressing, but it is essential to recognize that help and effective management strategies are available. In this article, we will explore bowel incontinence, its causes, diagnosis, treatment options, and practical tips for coping with this condition.
Understanding Bowel Incontinence
Bowel incontinence can vary in severity, ranging from occasional leakage of gas to the complete loss of control over stool. It can affect people of all ages, but it is more common in older adults. This condition can result from various factors that affect the muscles and nerves responsible for bowel control.
Causes of Bowel Incontinence
- Muscle Weakness: Weakness or damage to the anal sphincter muscles, which control the release of stool, can lead to bowel incontinence. Childbirth, trauma, or surgery can contribute to muscle weakness.
- Nerve Damage: Conditions like diabetes, multiple sclerosis, and spinal cord injuries can damage the nerves that regulate bowel movements, impairing sensation and control.
- Chronic Constipation: Long-term constipation can stretch and damage the rectum, reducing its ability to sense stool and hold it until an appropriate time.
- Diarrhea: Chronic diarrhea or conditions like irritable bowel syndrome (IBS) can make it difficult to control bowel movements.
- Rectal Prolapse: When the rectum protrudes from the anus, it can disrupt normal bowel control.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can cause inflammation and damage to the intestinal lining, affecting bowel control.
here are key points explaining the causes of bowel incontinence:
- Muscle Weakness: One of the primary causes of bowel incontinence is weakness or damage to the muscles that control the rectum and anus. These muscles, known as the anal sphincter muscles, play a crucial role in holding stool in the rectum until you are ready to have a bowel movement. Factors like childbirth, trauma during childbirth, or surgical procedures in the pelvic area can weaken or damage these muscles.
- Nerve Damage: Damage to the nerves that regulate bowel movements can result in bowel incontinence. Conditions like diabetes, multiple sclerosis, and spinal cord injuries can affect the nerves responsible for sensing when the rectum is full and coordinating the muscles required for bowel control.
- Chronic Constipation: Persistent and untreated constipation can lead to bowel incontinence. Over time, chronic constipation can stretch and damage the rectum, making it less responsive to the normal signals that indicate when it’s time to have a bowel movement.
- Diarrhea: Frequent or chronic diarrhea can contribute to bowel incontinence. It can overwhelm the rectum’s ability to contain stool, leading to leakage or urgency.
- Rectal Prolapse: In some cases, a condition known as rectal prolapse can cause bowel incontinence. This occurs when the rectum protrudes from the anus, disrupting normal bowel control.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis, which fall under the umbrella of inflammatory bowel disease, can cause inflammation and damage to the intestinal lining. This damage can impair bowel control.
- Surgery: Surgical procedures involving the rectum, colon, or pelvic area can sometimes damage the nerves or muscles responsible for bowel control, resulting in bowel incontinence.
- Radiation Therapy: Radiation therapy used to treat certain cancers in the pelvic region can damage healthy tissue, including the muscles and nerves involved in bowel control.
- Medications: Certain medications, especially laxatives or antidiarrheal drugs, can potentially contribute to bowel incontinence if not used appropriately.
It’s important to note that bowel incontinence can have multiple contributing factors, and in some cases, the exact cause may be a combination of these factors. Accurate diagnosis and identification of the underlying causes are essential for developing an effective treatment plan to manage bowel incontinence. Consulting a healthcare professional is crucial for individuals experiencing this condition.
Diagnosis of Bowel Incontinence
If you suspect you have bowel incontinence, it is crucial to consult a healthcare professional. They will conduct a thorough evaluation, which may include:
- Medical History: Your healthcare provider will ask about your symptoms, medical history, and any underlying conditions.
- Physical Examination: A physical examination may help identify any physical factors contributing to the condition.
- Anal Manometry: This test measures the pressure in the rectum and anal sphincter muscles, helping to assess muscle strength and function.
- Endoscopy: In some cases, a flexible tube with a camera (endoscope) may be used to examine the rectum and lower colon for abnormalities.
- Stool Testing: Stool samples may be examined to rule out infections or other gastrointestinal issues.
Treatment and Management
Treatment options for bowel incontinence depend on the underlying causes and severity of the condition. These may include:
- Dietary Changes: Adjusting your diet to manage diarrhea or constipation can help improve bowel control. Fiber supplements, increased fluid intake, and avoiding trigger foods can be beneficial.
- Medications: Medications may be prescribed to manage diarrhea, constipation, or underlying conditions like IBD.
- Pelvic Floor Exercises: Physical therapy and exercises can help strengthen the pelvic floor muscles, improving bowel control.
- Biofeedback: Biofeedback therapy can teach individuals how to control and strengthen their pelvic muscles using visual and sensory cues.
- Surgery: In severe cases, surgical options may be considered, such as sphincter repair or placement of a colostomy or artificial sphincter.
Coping Strategies for Bowel Incontinence
Coping with bowel incontinence can be emotionally challenging, but there are practical strategies to help manage the condition:
- Use Absorbent Products: Disposable pads or adult diapers can provide peace of mind and help manage leakage.
- Maintain Good Hygiene: Proper hygiene, including regular cleansing and use of barrier creams, can prevent skin irritation and discomfort.
- Create a Bathroom Schedule: Establishing a regular bathroom routine can help reduce the risk of accidents.
- Dietary Awareness: Be mindful of foods that trigger symptoms and try to identify and avoid them.
- Open Communication: Talk to your healthcare provider about your experiences and any concerns or questions you may have. Support groups and counseling can also provide emotional support.
Conclusion
Bowel incontinence is a challenging condition, but it is important to remember that you are not alone, and effective management strategies are available. Seeking medical advice and exploring treatment options can help improve your quality of life and enable you to regain control over your bowel movements. Additionally, connecting with healthcare professionals, support groups, and loved ones can provide valuable emotional support on your journey towards better bowel control.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023