Cavus Foot: Understanding, Managing, and Thriving
Introduction:
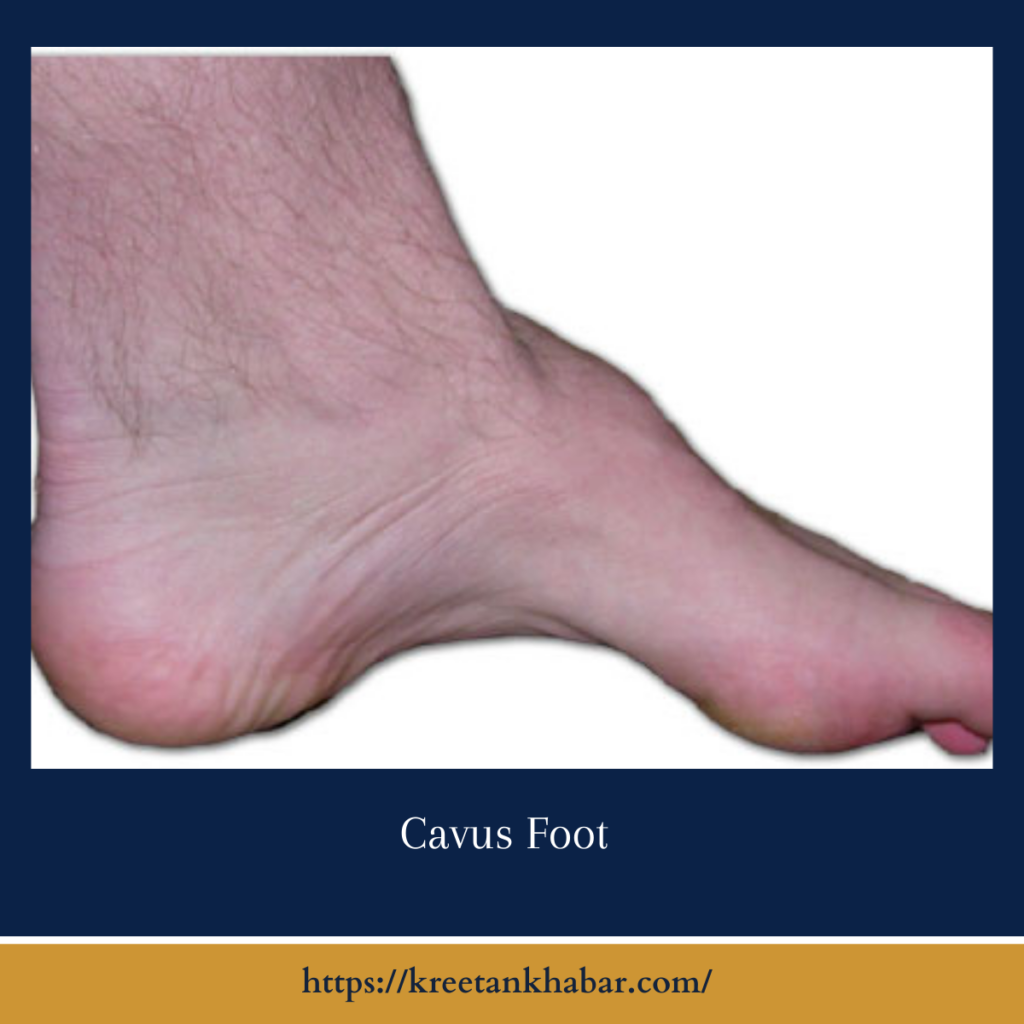
In the intricate realm of podiatric health, the cavus foot stands as a unique entity, often overshadowed by its more commonly recognized counterpart, flat feet. However, this high-arched condition, known as pes cavus or cavus foot, presents its own set of challenges and complexities. From understanding its characteristics to exploring management strategies, this article aims to shed light on the intricacies of cavus foot, offering insights into diagnosis, treatment options, and tips for living well with this condition.
Understanding Cavus Foot:
Cavus foot is characterized by an exaggerated arch along the length of the foot, resulting in increased weight-bearing on the ball and heel. Unlike flat feet, where the arch is collapsed or absent, cavus foot presents with a pronounced arch, often accompanied by clawed toes and a supinated foot position. This structural variation can lead to altered foot biomechanics, instability, and an increased risk of foot-related problems.
Causes and Risk Factors:
The causes and risk factors of cavus foot, also known as pes cavus, encompass a variety of genetic, neurological, and biomechanical influences. Genetic predisposition plays a significant role, with individuals often inheriting the condition from family members who exhibit a similar foot structure. Neurological disorders such as Charcot-Marie-Tooth disease, spinal cord lesions, or cerebral palsy can disrupt the normal function of muscles and nerves in the feet, leading to muscle imbalances and abnormal foot posture characteristic of cavus foot.
Muscular imbalances, whether due to weakness or tightness in the muscles of the foot and lower leg, can also contribute to the development of a high arch. Additionally, certain connective tissue disorders, including Ehlers-Danlos syndrome or Marfan syndrome, may predispose individuals to abnormal foot postures, further increasing the risk of developing cavus foot. These interconnected factors underscore the complex nature of cavus foot development, highlighting the importance of considering multiple influences when evaluating and managing this condition.
Several factors contribute to the development of cavus foot, including:
- Genetics: Hereditary predisposition plays a significant role, with individuals often inheriting the condition from family members.
- Neurological Disorders: Certain neurological conditions, such as Charcot-Marie-Tooth disease, spinal cord lesions, or cerebral palsy, can result in muscle imbalances and abnormal foot posture.
- Muscular Imbalances: Weakness or tightness in the muscles of the foot and lower leg can disrupt normal foot mechanics, leading to the development of a high arch.
- Connective Tissue Disorders: Conditions like Ehlers-Danlos syndrome or Marfan syndrome, which affect connective tissue integrity, may contribute to the development of cavus foot.
Symptoms and Complications:
Individuals with cavus foot may experience a range of symptoms and complications, including:
- Foot pain, particularly in the ball and heel areas, due to increased pressure.
- Instability and difficulty maintaining balance, leading to an increased risk of falls.
- Clawed toes or hammertoes, resulting from muscle imbalances and abnormal foot mechanics.
- Calluses and corns, which may develop on areas of increased pressure, such as the ball of the foot or the outside edge of the heel.
- Foot deformities, such as plantar fasciitis or stress fractures, secondary to altered foot biomechanics.
Management and Treatment Options:
Management and treatment options for cavus foot, also known as pes cavus, are diverse and tailored to address individual symptoms and underlying causes. Custom orthotic devices are commonly prescribed to provide support and stability, redistributing pressure and promoting proper foot alignment. These orthotics help alleviate pain, reduce instability, and improve overall foot function during weight-bearing activities. Physical therapy plays a crucial role in strengthening weak muscles, improving flexibility, and correcting muscle imbalances that contribute to cavus foot.
Targeted exercises aim to enhance foot biomechanics, restore range of motion, and prevent further complications. Additionally, footwear modifications such as choosing shoes with adequate arch support, cushioning, and stability are essential to accommodate the foot’s shape and alleviate pressure points. In severe cases or when conservative measures fail to provide relief, surgical intervention may be considered to correct structural abnormalities or release tight soft tissues. Surgical procedures, including tendon lengthening, osteotomy, or fusion, aim to stabilize the foot and improve overall function. Overall, a multidisciplinary approach involving podiatrists, physical therapists, and orthopedic surgeons is crucial for developing comprehensive treatment plans that address the diverse needs of individuals with cavus foot.
Managing cavus foot involves a comprehensive approach aimed at relieving symptoms, improving foot function, and preventing complications. Treatment options may include:
- Orthotic Devices: Custom-made orthotic inserts are designed to support the arch, redistribute pressure, and improve foot alignment. These devices help alleviate pain, reduce instability, and promote optimal foot biomechanics during walking or standing.
- Physical Therapy: Targeted exercises focusing on muscle strengthening, flexibility, and balance can help address underlying muscular imbalances and improve foot function. Stretching techniques may also be prescribed to alleviate tightness in the calf muscles and plantar fascia.
- Footwear Modifications: Choosing appropriate footwear with adequate arch support, cushioning, and stability is essential for individuals with cavus foot. Shoes with a wide toe box and a low heel can help accommodate the foot’s shape and reduce pressure points.
- Surgical Intervention: In severe cases of cavus foot or when conservative measures fail to provide relief, surgical intervention may be considered. Surgical procedures aim to correct structural abnormalities, release tight soft tissues, or stabilize the foot through fusion or osteotomy.
Living with Cavus Foot:
Living well with cavus foot requires proactive management, self-care, and awareness of potential complications. Individuals with pes cavus should:
- Monitor symptoms and seek medical attention for any changes or worsening of pain or instability.
- Adhere to prescribed treatment plans, including wearing orthotic devices, performing recommended exercises, and selecting appropriate footwear.
- Practice good foot hygiene and inspect the feet regularly for signs of irritation, blisters, or calluses.
- Engage in low-impact activities and exercises that are gentle on the feet while avoiding high-impact sports that may exacerbate symptoms.
Conclusion:
Cavus foot may present unique challenges, but with proper understanding, management, and support, individuals can effectively navigate the complexities of this condition and lead active, fulfilling lives. By addressing underlying factors, implementing tailored treatment strategies, and adopting proactive self-care practices, those with cavus foot can minimize discomfort, optimize foot function, and enhance overall quality of life.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023