Cerebral Cavernous Malformation: Understanding a Stealthy Brain Disorder
Introduction:
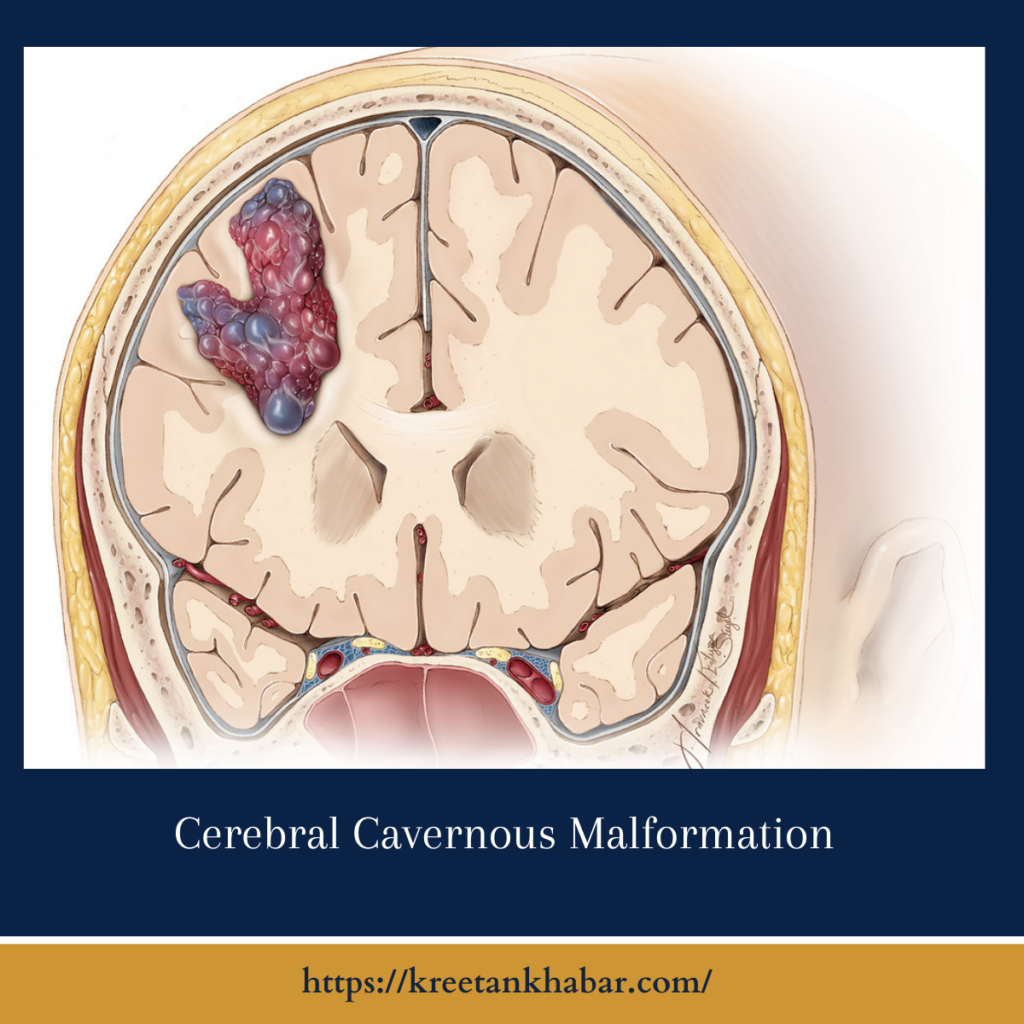
Cerebral cavernous malformation (CCM), also known as cavernous angioma or cavernoma, is a relatively rare but potentially serious vascular disorder affecting the brain and spinal cord. Despite its low prevalence, CCM can have significant neurological consequences if left undiagnosed or untreated. This article aims to unravel the mysteries surrounding CCM, shedding light on its pathogenesis, clinical manifestations, diagnosis, and management strategies.
The Enigmatic Pathogenesis:
The pathogenesis of cerebral cavernous malformation remains an area of active research, with significant strides made in recent years. CCM is primarily characterized by abnormally enlarged and irregularly shaped blood vessels, resembling small “caverns” or “cysts” filled with blood. These vascular abnormalities result from genetic mutations affecting genes such as CCM1, CCM2, and CCM3, which play crucial roles in endothelial cell function and blood vessel integrity. Disruption of these genes leads to weakened vessel walls, increased permeability, and susceptibility to hemorrhage, ultimately contributing to the formation of cavernous malformations.
Clinical Manifestations:
The clinical presentation of cerebral cavernous malformation can vary widely, ranging from asymptomatic incidental findings on imaging studies to severe neurological deficits and life-threatening hemorrhages. Common symptoms may include seizures, headaches, focal neurological deficits, such as weakness or sensory disturbances, and cognitive impairments. However, the clinical course of CCM is unpredictable, with some individuals remaining asymptomatic throughout their lives, while others experience recurrent hemorrhages or progressive neurological deterioration.
Diagnosis and Imaging:
Diagnosing cerebral cavernous malformation typically involves a combination of clinical evaluation and neuroimaging studies. Magnetic resonance imaging (MRI) is the gold standard for visualizing cavernous malformations, as it provides detailed anatomical information and can distinguish between active lesions and stable hemosiderin deposits. Advanced imaging techniques such as susceptibility-weighted imaging (SWI) and gradient echo sequences enhance the detection of small lesions and microhemorrhages, aiding in accurate diagnosis and treatment planning.
- Magnetic Resonance Imaging (MRI): MRI is the cornerstone imaging modality for diagnosing cerebral cavernous malformations (CCMs). It offers high-resolution anatomical details and superior soft tissue contrast, enabling the identification of characteristic cavernous lesions within the brain and spinal cord.
- Susceptibility-Weighted Imaging (SWI): SWI is a specialized MRI technique that enhances the detection of cerebral cavernous malformations by exploiting their unique susceptibility effects. This sensitive imaging method allows for the visualization of small lesions and microhemorrhages associated with CCMs, even in the absence of overt clinical symptoms.
- Gradient Echo Sequences: Gradient echo sequences, including T2*-weighted and susceptibility-weighted sequences, are particularly valuable in detecting hemosiderin deposits, a hallmark of chronic hemorrhage within cerebral cavernous malformations. These sequences provide crucial information about lesion stability and can aid in distinguishing between active lesions and old hemorrhages.
- Contrast-Enhanced MRI: While contrast-enhanced MRI is not typically required for diagnosing cerebral cavernous malformations, it may be utilized in specific cases to evaluate associated vascular abnormalities or to differentiate CCMs from other pathologies with similar radiographic features, such as tumors or arteriovenous malformations.
- Diffusion-Weighted Imaging (DWI): DWI is a functional MRI technique that measures the diffusion of water molecules within tissues, providing insights into tissue microstructure and integrity. Although not routinely used for diagnosing cerebral cavernous malformations, DWI may offer supplementary information in cases of acute hemorrhage or associated ischemic events.
- Magnetic Resonance Angiography (MRA): MRA is a non-invasive imaging technique that visualizes the blood vessels within the brain and can help identify any associated vascular abnormalities or anomalies in patients with cerebral cavernous malformations. While not essential for the primary diagnosis of CCMs, MRA may be performed to assess the overall vascular architecture and aid treatment planning.
- Computed Tomography (CT) Scans: While MRI is the preferred imaging modality for diagnosing cerebral cavernous malformations due to its superior soft tissue contrast, CT scans may be considered in certain clinical scenarios, such as acute hemorrhage or contraindications to MRI. However, CT imaging typically has lower sensitivity for detecting CCMs compared to MRI.
- Follow-Up Imaging: Given the unpredictable nature of cerebral cavernous malformations and the potential for lesion growth or hemorrhage over time, regular follow-up imaging with MRI is essential for monitoring disease progression and treatment response. Serial imaging studies enable clinicians to assess lesion stability, detect new lesions, and adjust management strategies accordingly.
- Multimodal Imaging Approach: A multimodal imaging approach, combining various MRI sequences and functional imaging techniques, enhances diagnostic accuracy and provides comprehensive information about cerebral cavernous malformations. By integrating different imaging modalities, clinicians can obtain a more nuanced understanding of CCMs and optimize patient care.
- Radiologist Expertise: Interpretation of imaging studies for cerebral cavernous malformations requires expertise in neuroimaging and familiarity with the characteristic radiographic features of CCMs. Collaboration with experienced neuroradiologists is essential to ensure accurate diagnosis, appropriate treatment planning, and optimal patient outcomes.
Management Strategies:
The management of cerebral cavernous malformation is multifaceted and tailored to individual patient characteristics, including lesion location, size, and clinical presentation. In asymptomatic cases or those with mild symptoms, a conservative approach with close observation and periodic imaging surveillance may be appropriate. However, for symptomatic or high-risk patients, treatment options may include seizure management with antiepileptic drugs, symptomatic relief of headaches, and surgical intervention to resect or obliterate symptomatic lesions. Emerging therapies targeting the underlying molecular pathways involved in CCM pathogenesis, such as anti-angiogenic agents and gene therapy, hold promise for future treatment advances.
Prognosis and Follow-Up:
The prognosis of cerebral cavernous malformation varies depending on several factors, including the number and location of lesions, history of hemorrhage, and presence of comorbidities. While some individuals may experience stable disease with minimal or no symptoms, others may face recurrent hemorrhages, progressive neurological decline, or complications related to surgical intervention. Regular follow-up with neurologists and neurosurgeons is essential for monitoring disease progression, adjusting treatment strategies as needed, and providing support to patients and their families.
Conclusion:
Cerebral cavernous malformation is a complex neurological disorder characterized by abnormal blood vessel formation in the brain and spinal cord. Despite its enigmatic pathogenesis and variable clinical course, advancements in genetic research and neuroimaging have improved our understanding of CCM and expanded treatment options for affected individuals. With continued research efforts and multidisciplinary collaboration, we strive to unravel the mysteries of this condition, improve diagnostic accuracy, and develop more effective therapies to enhance the quality of life for patients living with cerebral cavernous malformation.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023