Cervical Cancer: A Preventable Threat Worth Understanding
Cervical cancer (also called as mixed carcinoma) is a significant public health concern that affects women worldwide. However, what sets it apart from many other cancers is its potential for prevention and early detection through regular screenings. In this article, we’ll explore cervical cancer in depth, covering its causes, risk factors, symptoms, screening methods, treatment options, and the importance of vaccination and awareness.
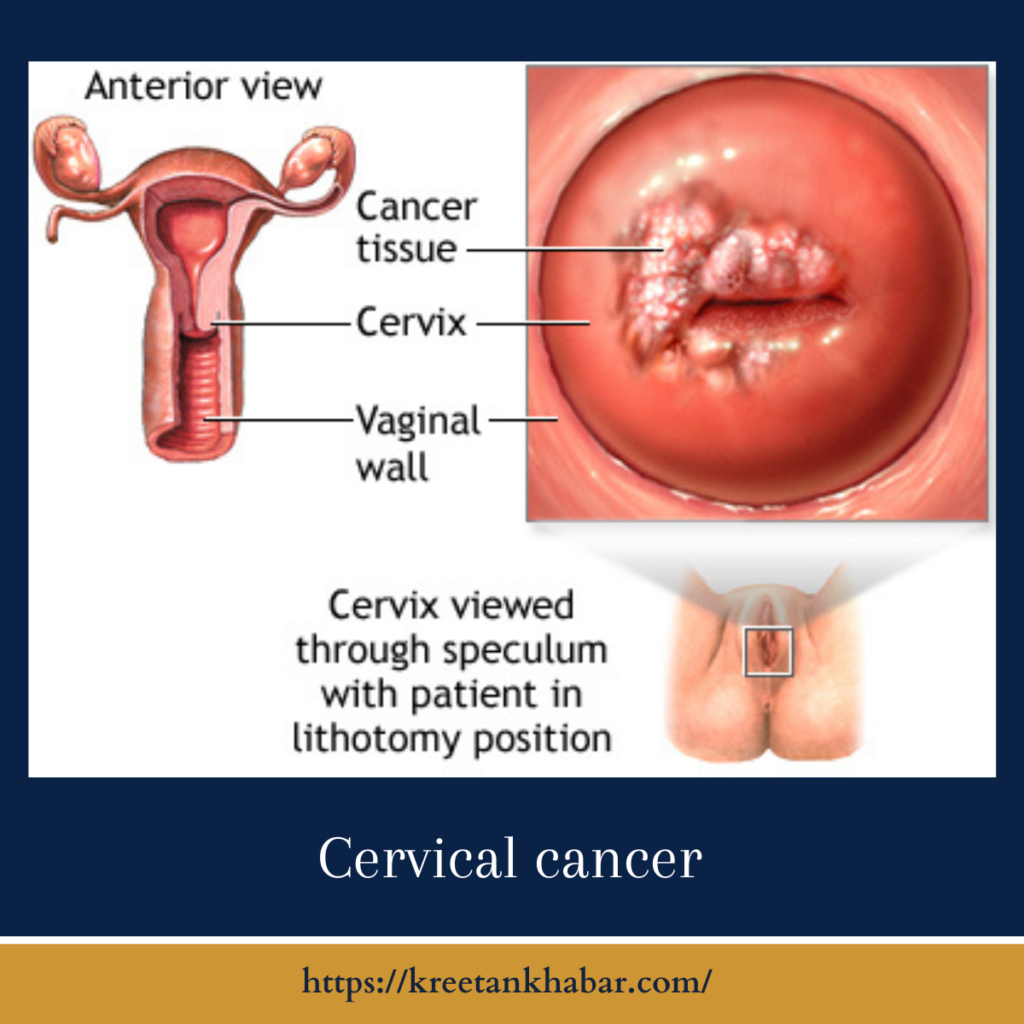
Understanding Cervical Cancer
Cervical cancer develops in the cervix, the narrow passage that connects the lower part of the uterus to the vagina. Most cervical cancers are caused by the human papillomavirus (HPV), a common sexually transmitted infection. It typically takes several years for cervical cells to develop into cancer, which presents a window of opportunity for early detection and intervention.
Risk Factors for Cervical Cancer
Several factors can increase the risk of developing cervical cancer:
- HPV Infection: Persistent infection with high-risk HPV strains is the primary cause of mixed carcinoma.
- Lack of HPV Vaccination: Vaccination against HPV is highly effective in preventing mixed carcinoma. Not receiving the vaccine increases the risk.
- Smoking: Smoking can increase the likelihood of developing mixed carcinoma in women with HPV infections.
- Weak Immune System: A weakened immune system, such as in individuals with HIV or those taking immunosuppressive medications, can make it harder for the body to fight off HPV infections.
- Early Sexual Activity: Engaging in sexual activity at a young age or having multiple sexual partners can increase the risk of HPV exposure.
- Low Socioeconomic Status: Limited access to healthcare and preventive measures can lead to a higher risk of mixed carcinoma.
Signs and Symptoms
Cervical cancer may not cause noticeable symptoms in its early stages, which is why regular screenings are crucial. As it progresses, symptoms can include:
- Abnormal Vaginal Bleeding: This includes bleeding between periods, after intercourse, or after menopause.
- Pelvic Pain: Pain during intercourse or pelvic pain not related to menstruation can be a symptom.
- Vaginal Discharge: Unusual vaginal discharge that may be foul-smelling or contain blood can occur.
Screening and Early Detection
Regular cervical cancer screening, typically done through a Pap smear or HPV test, is essential for early detection. These tests can identify abnormal cervical cell changes long before they become cancerous. Early detection allows for effective treatment and higher chances of survival.
Treatment Options
The treatment of cervical cancer depends on the stage at which it is diagnosed. Common treatment options include:
- Surgery: Surgical procedures may involve removing the cancerous tissue or, in more advanced cases, a hysterectomy (removal of the uterus).
- Radiation Therapy: Radiation can target and destroy cancer cells in the cervix and nearby areas.
- Chemotherapy: Chemotherapy may be used in combination with other treatments to kill cancer cells or shrink tumors.
- Targeted Therapy: Targeted drugs can block specific molecules involved in cancer growth and progression.
Prevention and Vaccination
Preventing cervical cancer is possible through a few key strategies:
- HPV Vaccination: The HPV vaccine is highly effective in preventing infections with the most common cancer-causing HPV strains. It is recommended for both boys and girls starting at an early age.
- Regular Screenings: Routine Pap smears and HPV tests for sexually active women can catch precancerous changes early.
- Safe Sex Practices: Reducing the number of sexual partners and using barrier methods, like condoms, can lower the risk of HPV transmission.
Prevention and Vaccination for Cervical Cancer: Key Points to Consider
- HPV Vaccination is Crucial: The human papillomavirus (HPV) vaccine is a powerful tool in preventing cervical cancer. It’s highly effective in protecting against the most common cancer-causing HPV strains.
- Recommended Age for Vaccination: HPV vaccination is recommended for both boys and girls, ideally between the ages of 9 and 12. It can be administered up to age 26 for individuals who haven’t been vaccinated earlier.
- Two- or Three-Dose Regimen: The vaccine is typically administered in a series of two or three doses, depending on the age at which vaccination begins.
- Herd Immunity: Widespread HPV vaccination not only protects individuals but also contributes to herd immunity, reducing the overall prevalence of HPV in the population.
- Safe Sex Practices: While vaccination is essential, practicing safe sex through condom use can provide an additional layer of protection against HPV and other sexually transmitted infections (STIs).
- Regular Screenings: Even vaccinated individuals should continue to undergo regular cervical cancer screenings, such as Pap smears and HPV tests. Vaccination does not cover all cancer-causing HPV strains.
- Screening Age and Frequency: The recommended age to start cervical cancer screenings may vary by country, but it’s typically around age 21. The frequency of screenings may decrease for vaccinated individuals with normal results.
- Behavioral Education: Education on the importance of safe sex, HPV vaccination, and regular screenings should be widely disseminated to raise awareness and encourage preventive actions.
- Access to Healthcare: Ensuring access to healthcare services, including vaccination and screenings, is vital for reaching underserved populations and reducing disparities in cervical cancer prevention.
- Global Efforts: Cervical cancer prevention efforts should extend globally, with a focus on countries with limited access to healthcare resources and vaccination programs.
- Public Health Campaigns: Government and healthcare organizations should launch public health campaigns to promote HPV vaccination and regular screenings.
- Parental Education: Parents and guardians should be informed about the importance of HPV vaccination for their children and encouraged to follow vaccination schedules.
- Community Outreach: Community-based programs and outreach efforts can help reach individuals who may not have easy access to healthcare facilities.
In summary, cervical cancer prevention relies heavily on HPV vaccination, safe sex practices, and regular screenings. Combining these strategies with education and awareness campaigns can significantly reduce the incidence of cervical cancer and save lives. Everyone, from healthcare providers to individuals and families, has a role to play in promoting prevention and vaccination against this preventable cancer.
Conclusion
Cervical cancer is a largely preventable and treatable disease when detected early. Regular screenings, HPV vaccination, and safe sex practices are crucial components of cervical cancer prevention. Awareness, education, and access to healthcare services play a pivotal role in reducing the burden of cervical cancer on women’s health globally. By taking proactive steps and encouraging others to do the same, we can work towards a world where cervical cancer becomes a rarity rather than a threat.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023