Cervical Dysplasia: Causes, Diagnosis, and Treatment Options
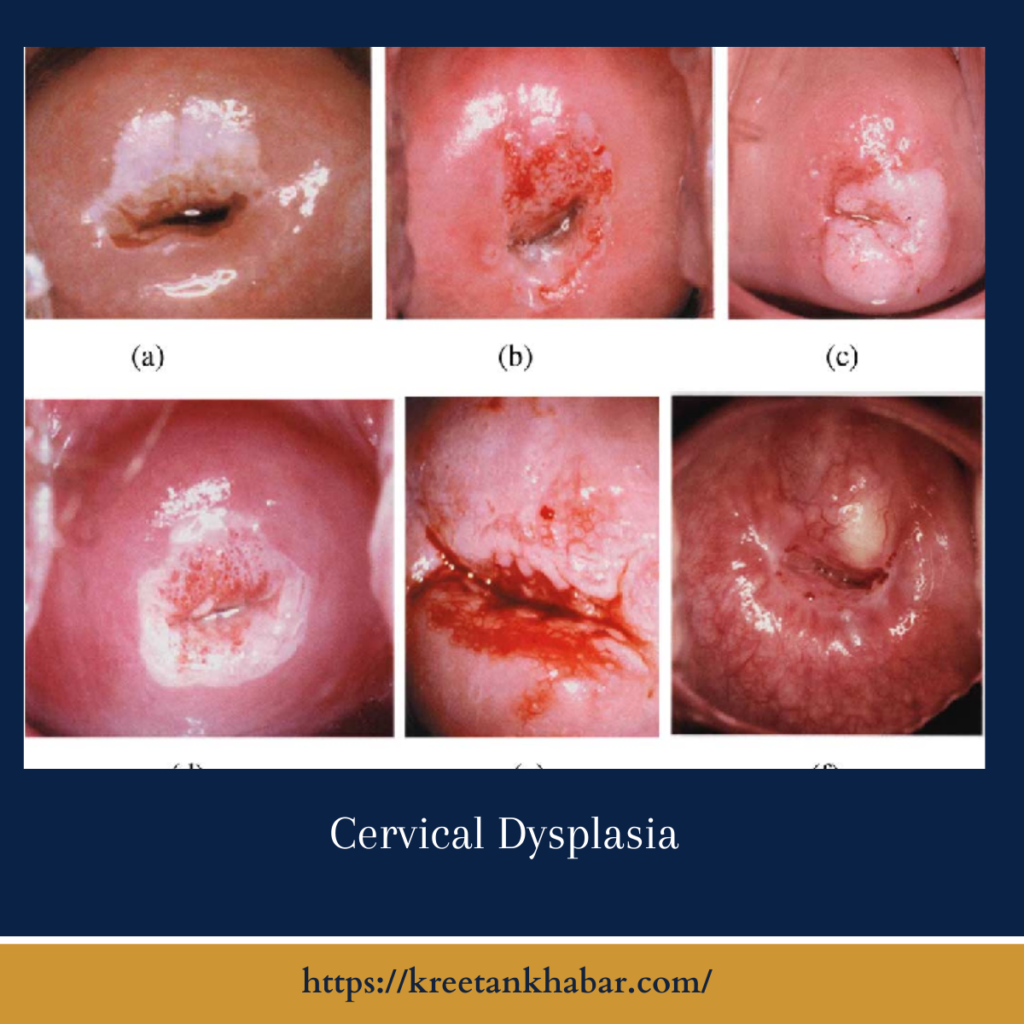
Cervical dysplasia(also known as spasmodic torticollis) is a condition characterized by abnormal changes in the cells lining the cervix, the lower part of the uterus that connects to the vagina. These changes are typically detected through routine cervical cancer screening tests, such as Pap smears or HPV tests. While cervical dysplasia itself is not cancerous, it is considered a precancerous condition and can increase the risk of developing cervical cancer if left untreated. In this article, we’ll explore the causes, diagnosis, and treatment options for cervical dysplasia to help individuals better understand this condition and navigate their healthcare journey.
Causes:
The primary cause of spasmodic torticollis is infection with certain types of human papillomavirus (HPV), a common sexually transmitted infection. HPV infection is incredibly common, with most sexually active individuals contracting the virus at some point in their lives. While the majority of HPV infections clear up on their own without causing any symptoms or long-term complications, persistent infection with high-risk strains of HPV can lead to the development of cervical dysplasia and, ultimately, cervical cancer. Other factors that may increase the risk of cervical dysplasia include smoking, a weakened immune system, and certain sexual behaviors.
Diagnosis:
Cervical dysplasia is typically diagnosed through routine cervical cancer screening tests, such as Pap smears or HPV tests. During a Pap smear, a healthcare provider collects a sample of cells from the cervix, which is then examined under a microscope for any abnormalities. An HPV test, on the other hand, detects the presence of high-risk strains of HPV in cervical cells. If abnormal cells are detected during screening, further diagnostic tests, such as colposcopy and cervical biopsy, may be performed to assess the extent of the abnormalities and determine the appropriate course of action.
Treatment Options:
The treatment approach for spasmodic torticollis depends on the severity of the abnormalities detected, as well as other individual factors such as age, overall health, and reproductive goals. In many cases, mild to moderate cervical dysplasia may resolve on its own without intervention, particularly in younger individuals with a healthy immune system. However, close monitoring and follow-up with healthcare providers are essential to ensure that any changes are promptly addressed.
For more significant or persistent cases of spasmodic torticollis, treatment options may include:
- Cryotherapy: Cryotherapy involves freezing abnormal cervical cells using a probe inserted into the cervix. This procedure destroys the abnormal cells and promotes the growth of healthy new cells in their place.
- Loop Electrosurgical Excision Procedure (LEEP): LEEP is a surgical procedure that uses a thin wire loop heated by electrical current to remove abnormal cervical tissue. This procedure is typically performed under local anesthesia and can be done in a healthcare provider’s office or outpatient setting.
- Cone biopsy: In cases of more severe spasmodic torticollis or when other treatment options are not effective, a cone biopsy may be recommended. This surgical procedure involves removing a cone-shaped piece of tissue from the cervix for further examination and treatment.
- Hysterectomy: In rare cases of advanced cervical dysplasia or when other treatments have failed, a hysterectomy may be recommended to remove the uterus and cervix entirely. This procedure is typically reserved for older individuals who have completed childbearing and have a high risk of developing cervical cancer.
In addition to these treatment options, individuals with cervical dysplasia are often advised to make lifestyle changes to reduce their risk of recurrence and progression, such as quitting smoking, practicing safe sex, and receiving the HPV vaccine if eligible.
In conclusion
cervical dysplasia is a common precancerous condition characterized by abnormal changes in the cells lining the cervix. While it can be concerning to receive a diagnosis of cervical dysplasia, it’s essential to remember that early detection and appropriate management can significantly reduce the risk of developing cervical cancer. By understanding the causes, diagnosis, and treatment options for cervical dysplasia, individuals can take proactive steps to protect their cervical health and overall well-being. Regular cervical cancer screening tests and open communication with healthcare providers are essential for early detection and optimal management of cervical dysplasia.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023