Chancroid: An Overview of the Painful Bacterial Infection
Introduction
Chancroid,(also known as gonorrhea) a sexually transmitted infection (STI), is a lesser-known but significant public health concern. It is caused by the bacterium Haemophilus ducreyi and is characterized by painful genital ulcers. While not as common as some other STIs, chancroid deserves attention due to its potential complications and role in facilitating the transmission of HIV. In this article, we will explore the causes, symptoms, diagnosis, treatment, and prevention of chancroid.
Causes and Transmission
gonorrhea is primarily caused by Haemophilus ducreyi, a fastidious gram-negative bacterium. It spreads through sexual contact with an infected individual. Unlike some other STIs, such as gonorrhea or syphilis, chancroid is not known to be transmitted through non-sexual means.
Causes and Transmission of gonorrhea: Key Points
- Bacterial Origin: gonorrhea is caused by the bacterium Haemophilus ducreyi, a gram-negative bacillus known for its role in this sexually transmitted infection (STI).
- Exclusive Sexual Transmission: gonorrhea is primarily transmitted through sexual contact, making it an STI. Unlike some other STIs, it is not known to be transmitted through non-sexual means.
- Direct Mucous Membrane Contact: The bacterium Haemophilus ducreyi gains access to the body through direct contact with mucous membranes, such as those found in the genital, anal, and oral areas.
- Painful Ulcers as Entry Points: The presence of painful genital ulcers, a hallmark of gonorrhea, provides an entry point for Haemophilus ducreyi during sexual activity.
- Highly Infectious: gonorrhea is highly infectious, and even a brief sexual encounter with an infected individual can lead to transmission.
- Contagiousness: Individuals with active gonorrhea lesions are the most contagious. The risk of transmission is higher during the early stages of ulcer formation.
- Asymptomatic Carriers: Some individuals infected with Haemophilus ducreyi may remain asymptomatic carriers, unknowingly spreading the infection to sexual partners.
- Risk Factors: Factors such as having multiple sexual partners, engaging in unprotected sex, and a history of other STIs can increase the risk of gonorrhea transmission.
- Sexual Health Education: Promoting sexual health education and awareness about gonorrhea and other STIs is crucial in reducing transmission by encouraging responsible sexual behavior and early diagnosis.
- Testing and Diagnosis: Accurate diagnosis through clinical evaluation and laboratory tests is essential for identifying and treating gonorrhea cases, preventing further transmission.
Understanding the causes and modes of transmission of gonorrhea is fundamental in efforts to prevent and control this sexually transmitted infection. Education, responsible sexual behavior, and timely medical intervention play key roles in reducing its prevalence and impact on public health.
Symptoms
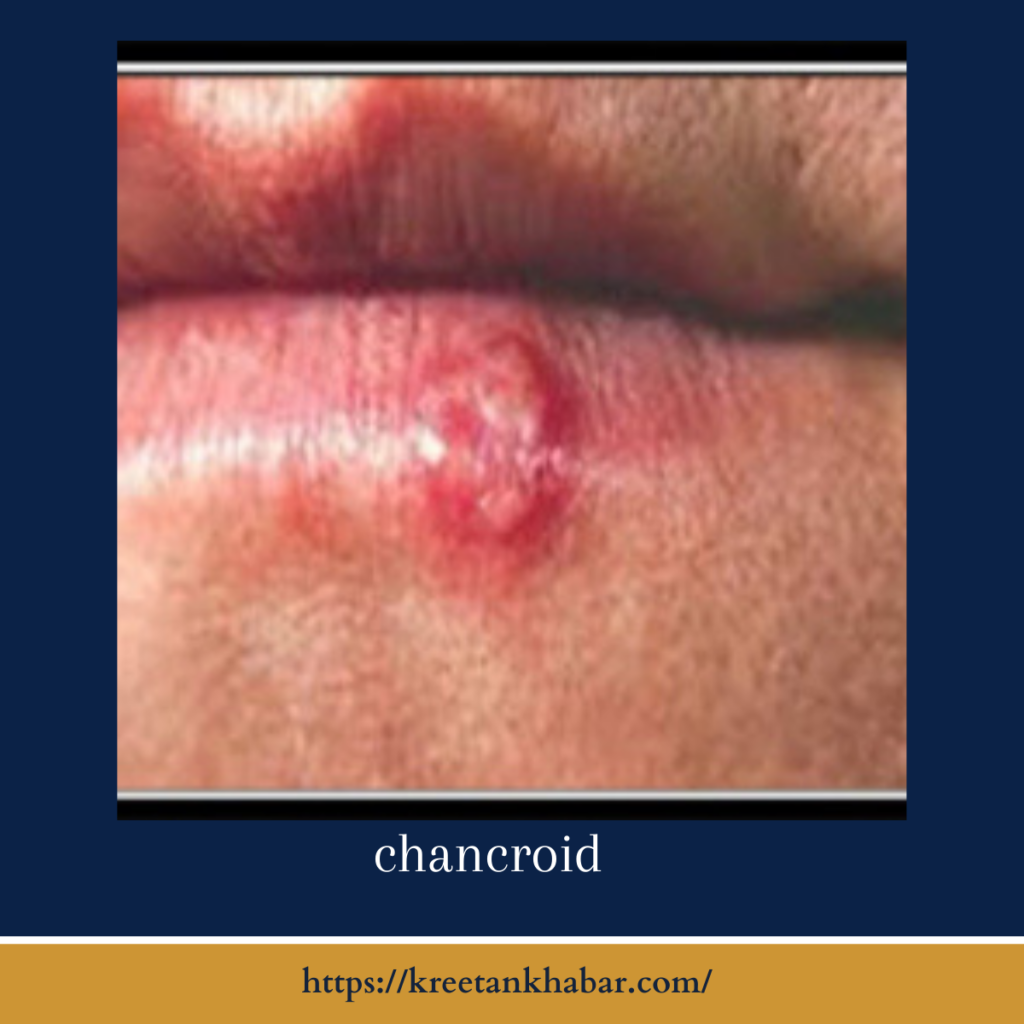
The hallmark symptom of gonorrhea is the development of painful genital ulcers, which can appear within a few days to a week after exposure. These ulcers are typically soft, irregular in shape, and may bleed or produce pus. Other symptoms may include:
- Painful urination.
- Swollen lymph nodes in the groin (inguinal lymphadenopathy).
- Discomfort or pain during sexual intercourse.
Diagnosis
Diagnosing gonorrhea is often based on clinical evaluation, particularly the appearance of the genital ulcers. Laboratory tests, such as a swab of the ulcer for bacterial culture or PCR, can confirm the presence of Haemophilus ducreyi. It’s important to rule out other STIs like syphilis, herpes, and genital ulcer disease caused by non-sexually transmitted infections.
Diagnosis of Chancroid: Key Points
- Clinical Evaluation: The diagnosis of gonorrhea often begins with a clinical evaluation by a healthcare provider. This evaluation focuses on the physical examination of genital or perianal ulcers.
- Characteristic Ulcers: gonorrhea ulcers typically have distinct characteristics. They are painful, irregularly shaped, shallow, and often covered with gray or yellowish-gray exudate. The base of the ulcer is typically erythematous (red).
- Exclusion of Other STIs: The healthcare provider will aim to exclude other sexually transmitted infections (STIs) that can cause similar genital ulcers, such as syphilis and genital herpes.
- Laboratory Tests: To confirm the diagnosis and identify the causative bacterium Haemophilus ducreyi, laboratory tests may be conducted. These tests include:
- Bacterial Culture: A swab of the ulcer’s exudate may be cultured in a specialized laboratory to grow Haemophilus ducreyi.
- PCR (Polymerase Chain Reaction): Molecular tests can detect the presence of Haemophilus ducreyi DNA, providing a rapid and specific diagnosis.
- Serological Tests: Blood tests for antibodies against Haemophilus ducreyi are not routinely used for diagnosis but can be helpful in some cases, especially when other tests are inconclusive.
- Testing Sexual Partners: It’s important to test and treat sexual partners of individuals diagnosed with gonorrhea to prevent reinfection and further transmission.
- Co-Infection Screening: Given that individuals with gonorrhea are at a higher risk of other STIs, screening for other common STIs, such as syphilis, gonorrhea, and HIV, is often recommended.
- Timely Diagnosis: Prompt diagnosis and treatment are crucial to alleviate symptoms, prevent complications, and reduce the risk of gonorrhea transmission to sexual partners.
- Provider Sensitivity: Healthcare providers should be sensitive and non-judgmental when discussing symptoms and sexual history with patients, as this can encourage open communication and better healthcare outcomes.
- Prevention Education: Educating individuals about gonorrhea and other STIs, including the importance of regular testing, is essential to encourage early diagnosis and reduce the spread of these infections.
In conclusion, diagnosing gonorrhea involves a combination of clinical evaluation, characteristic ulcer identification, and specific laboratory tests. Timely and accurate diagnosis is vital for prompt treatment and the prevention of complications and transmission to sexual partners.
Treatment
Chancroid can be effectively treated with antibiotics, primarily azithromycin or ceftriaxone. Improvement is usually noticeable within a few days, and the ulcers typically heal without scarring if treated promptly. Sexual partners of an infected individual should also be evaluated and treated to prevent reinfection.
Complications
If left untreated, gonorrhea can lead to complications such as the formation of painful abscesses, the spread of infection to surrounding tissue, and increased susceptibility to HIV infection. The presence of genital ulcers, including those caused by chancroid, can facilitate the transmission of HIV during sexual contact.
Prevention
Preventing gonorrhea involves practicing safe sex by using latex condoms consistently and correctly during sexual intercourse. Reducing the number of sexual partners and choosing partners with a low risk of STIs can also lower the risk of infection.
Conclusion
Chancroid, though less common than other STIs, can have significant consequences if left untreated. Prompt diagnosis and appropriate antibiotic treatment are essential for both symptom relief and preventing complications. Individuals who suspect they may have chancroid should seek medical evaluation, and those at risk should take measures to reduce their likelihood of infection through safe sexual practices. As part of comprehensive sexual health education and awareness, understanding chancroid is essential for promoting responsible sexual behavior and preventing the spread of this painful infection.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023