Charcot-Marie-Tooth Disease: Understanding the Genetics, Symptoms, and Management
Charcot-Marie-Tooth disease (CMT), named after the three physicians who first described it in 1886, is one of the most common inherited neurological disorders affecting the peripheral nerves. This group of disorders encompasses a heterogeneous spectrum of genetic mutations that lead to progressive damage to the peripheral nerves, resulting in muscle weakness, sensory loss, and various neurological symptoms. Despite its prevalence, Charcot-Marie-Tooth disease remains relatively unfamiliar to many, underscoring the importance of raising awareness and understanding about this complex condition.
The Genetic Basis of CMT:
CMT is primarily a genetic disorder, with most cases being inherited in an autosomal dominant pattern, although autosomal recessive and X-linked forms also exist. Mutations in genes encoding proteins involved in the structure and function of peripheral nerves, such as myelin sheath formation, axonal transport, and nerve cell signaling, underlie the pathogenesis of Charcot-Marie-Tooth disease. Over 100 different genes have been implicated in Charcot-Marie-Tooth disease, contributing to its clinical heterogeneity and variability in symptom presentation.
Clinical Manifestations and Symptoms:
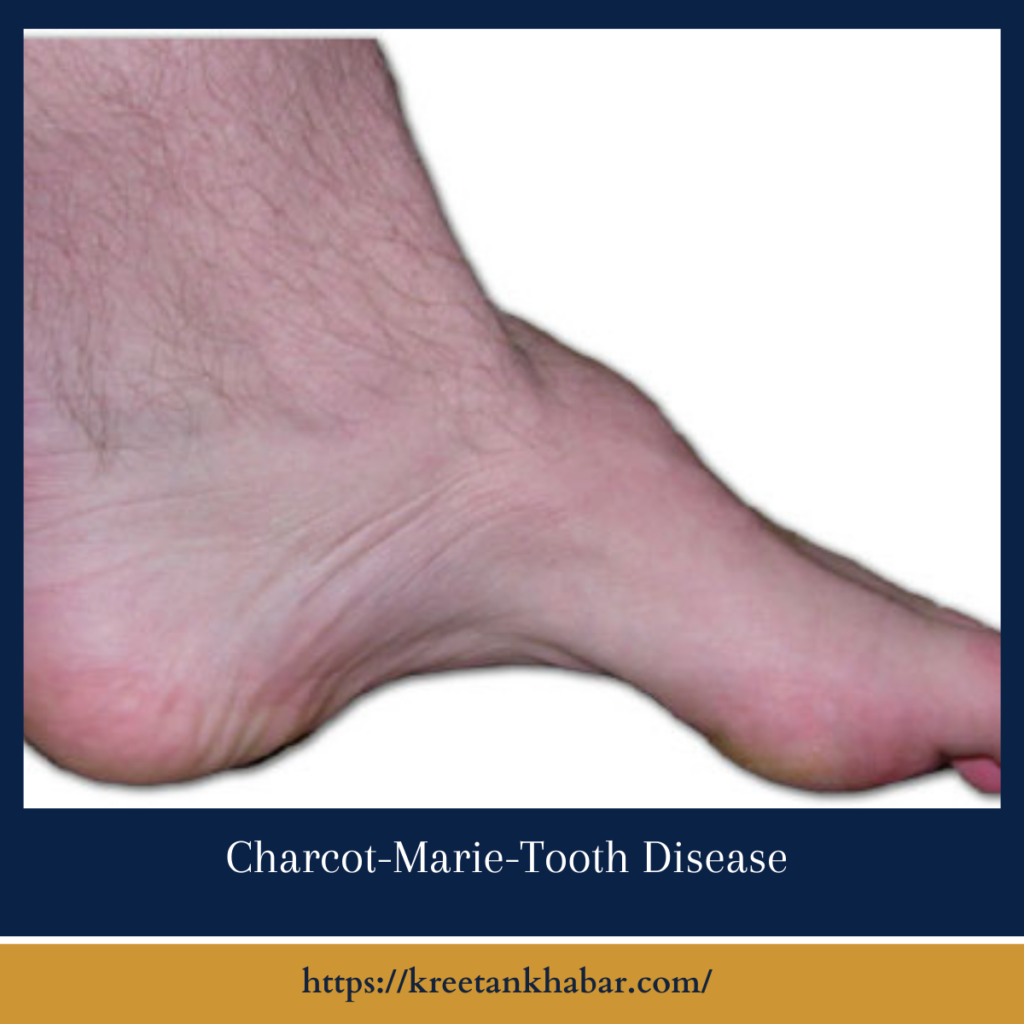
The hallmark features of Charcot-Marie-Tooth disease include progressive muscle weakness and wasting, predominantly affecting the distal muscles of the lower limbs and feet. This leads to characteristic foot deformities such as high arches (pes cavus) and hammertoes, as well as difficulty walking and maintaining balance. Sensory symptoms, including numbness, tingling, and decreased sensation in the extremities, are also common, along with diminished reflexes and muscle cramps. In severe cases, individuals may experience hand weakness, difficulty with fine motor tasks, and impaired sensation in the hands and fingers.
Diagnosis and Differential Diagnosis:
Diagnosing CMT often involves a combination of clinical evaluation, electromyography (EMG), nerve conduction studies, and genetic testing. Electrophysiological studies can help assess the extent of peripheral nerve involvement and distinguish between demyelinating (CMT1) and axonal (CMT2) forms of the disease. Genetic testing, including targeted gene panels and whole-exome sequencing, can identify specific genetic mutations associated with Charcot-Marie-Tooth disease, facilitating accurate diagnosis and classification. Differential diagnosis may include other causes of peripheral neuropathy, such as diabetic neuropathy, hereditary neuropathies, and acquired neuropathies secondary to infections or toxins.
Management and Treatment Strategies:
While there is currently no cure for Charcot-Marie-Tooth disease, management focuses on symptom relief, functional improvement, and minimizing complications. Treatment strategies may include:
- Physical Therapy: Exercise programs, stretching, and orthotic devices can help improve muscle strength, mobility, and gait stability, while also preventing contractures and deformities.
- Occupational Therapy: Adaptive devices, ergonomic tools, and assistive technology can assist individuals with activities of daily living, such as dressing, grooming, and fine motor tasks.
- Pain Management: Medications such as analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and anticonvulsants may be prescribed to alleviate neuropathic pain and discomfort.
- Surgical Interventions: In cases of severe deformity or functional impairment, surgical procedures such as tendon release, joint fusion, or corrective osteotomy may be considered to improve mobility and quality of life.
Research and Future Directions:
Advances in genetic testing technologies, molecular biology, and gene therapy hold promise for the future of Charcot-Marie-Tooth disease treatment and management. Ongoing research efforts seek to elucidate the underlying pathophysiological mechanisms, identify potential therapeutic targets, and develop novel treatment modalities aimed at slowing disease progression and improving outcomes for individuals with Charcot-Marie-Tooth disease. Collaborative initiatives involving researchers, clinicians, advocacy groups, and affected individuals are essential for driving innovation and advancing our understanding of this complex disorder.
Conclusion:
Charcot-Marie-Tooth disease is a complex neurological disorder characterized by progressive peripheral nerve damage, muscle weakness, and sensory abnormalities. While the disease poses significant challenges for affected individuals and their families, ongoing research and multidisciplinary care approaches offer hope for improved diagnosis, treatment, and management. By raising awareness, promoting early detection, and fostering collaborative research endeavors, we can empower individuals with Charcot-Marie-Tooth disease to live fulfilling lives and access the support and resources they need to navigate the complexities of this condition.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023