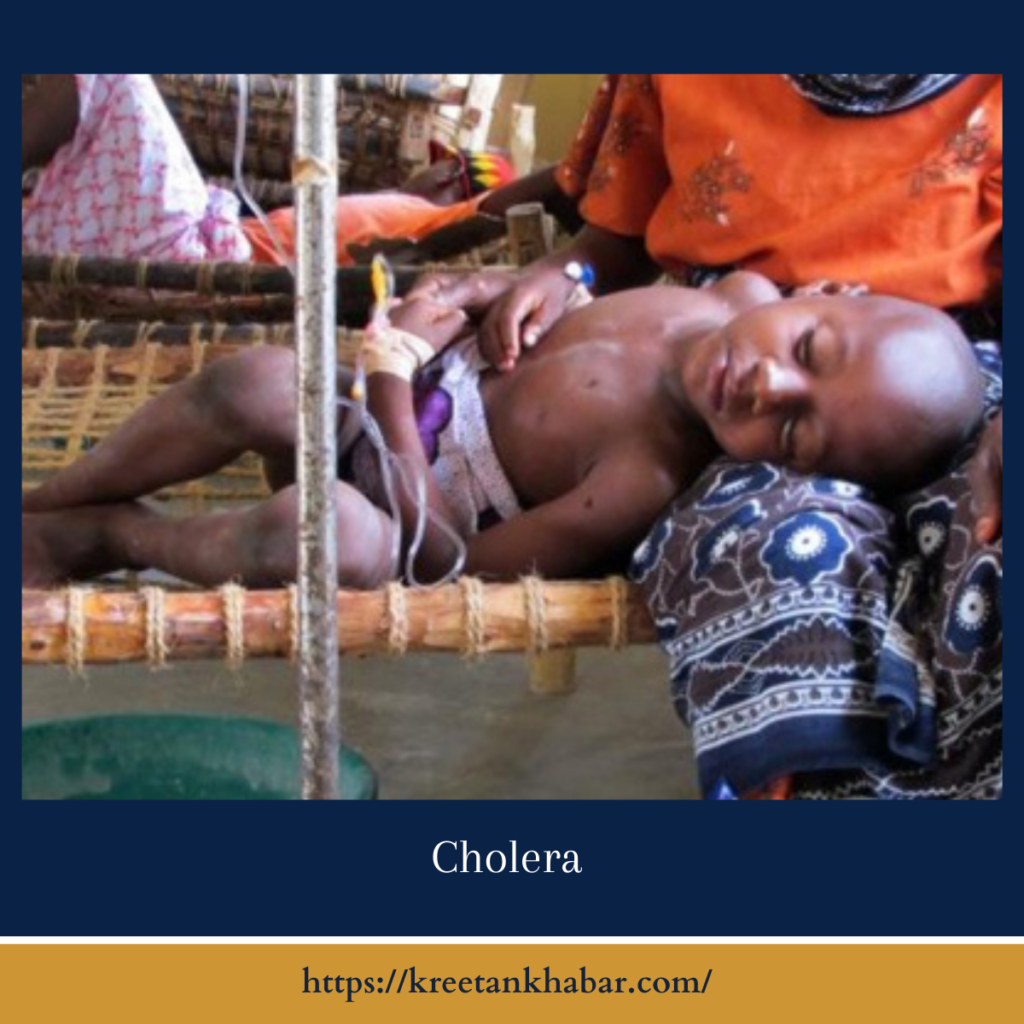
Cholera: Causes, Symptoms, Treatment, and Prevention
Cholera, a severe diarrheal illness caused by the bacterium Vibrio cholerae, has plagued human populations for centuries, particularly in regions with inadequate sanitation and access to clean water. While advancements in public health and sanitation have reduced the global burden of diarrheal illness, outbreaks still occur, posing a significant threat to communities, especially in areas affected by natural disasters or humanitarian crises. This article provides an overview of cholera, including its causes, symptoms, treatment, and prevention strategies.
Causes:
Cholera is primarily spread through the ingestion of contaminated food or water containing the Vibrio cholerae bacterium. The bacterium produces a toxin that causes the intestines to secrete large volumes of fluid, leading to profuse, watery diarrhea characteristic of diarrheal illness. Contaminated water sources, inadequate sewage disposal, and poor hygiene practices contribute to the transmission of diarrheal illness, particularly in areas with overcrowded living conditions or limited access to clean water and sanitation facilities. In regions prone to natural disasters or humanitarian emergencies, such as earthquakes or floods, the risk of cholera outbreaks is heightened due to disruption of infrastructure and displacement of populations.
Symptoms:
The symptoms of cholera can range from mild to severe and typically appear within a few hours to five days after exposure to the bacterium. The hallmark symptom of cholera is profuse, watery diarrhea, often described as “rice-water stool” due to its appearance. Diarrhea may be accompanied by vomiting, dehydration, muscle cramps, and rapid heart rate. Severe dehydration can lead to electrolyte imbalances, shock, and organ failure if left untreated. In some cases, individuals may experience no symptoms or only mild gastrointestinal discomfort, making it challenging to detect and control the spread of the disease.
- Rapid Onset of Profuse Diarrhea: Cholera is characterized by the sudden onset of severe diarrhea, often described as “rice-water stool” due to its pale, watery appearance. This diarrhea can be explosive and lead to rapid fluid loss, contributing to dehydration.
- Vomiting: Alongside diarrhea, individuals with diarrheal illness may experience episodes of vomiting, further exacerbating fluid and electrolyte imbalances. The combination of vomiting and diarrhea can quickly lead to dehydration and electrolyte disturbances.
- Dehydration: Dehydration is a hallmark feature of diarrheal illness and can develop rapidly due to the excessive fluid loss associated with diarrhea and vomiting. Symptoms of dehydration may include dry mouth, thirst, decreased urine output, and lethargy.
- Muscle Cramps: Cholera-induced dehydration can result in muscle cramps or spasms, particularly in the legs and abdomen. These cramps may be painful and contribute to discomfort and weakness in affected individuals.
- Rapid Heart Rate: Dehydration and electrolyte imbalances caused by diarrheal illness can lead to a rapid heart rate (tachycardia) as the body attempts to compensate for decreased blood volume and maintain adequate circulation.
- Sunken Eyes: Dehydration can cause the eyes to appear sunken or hollowed out, a characteristic sign of fluid loss and electrolyte disturbances commonly seen in severe cases of cholera.
- Cold, Clammy Skin: Individuals with cholera may develop cold, clammy skin as a result of dehydration and decreased blood flow to the skin’s surface. This can contribute to feelings of coldness or shivering despite normal ambient temperatures.
- Weakness and Fatigue: Dehydration and electrolyte imbalances associated with diarrheal illness can lead to weakness, fatigue, and lethargy. Individuals may feel drained of energy and unable to perform usual activities due to the effects of fluid loss and dehydration on the body.
- Thirst: Intense thirst is a common symptom of cholera, driven by the body’s need to replenish lost fluids. Despite drinking water or oral rehydration solutions, individuals may continue to feel thirsty as the body attempts to restore fluid balance.
- Confusion and Altered Mental Status: In severe cases of cholera, electrolyte disturbances and dehydration can affect brain function, leading to confusion, disorientation, and altered mental status. This can manifest as difficulty concentrating, irritability, or impaired consciousness.
Recognizing these symptoms is crucial for prompt diagnosis and treatment of diarrheal illness, particularly in areas where the disease is endemic or during outbreaks. Early intervention with oral rehydration therapy and appropriate medical care can help prevent complications and reduce the risk of mortality associated with severe cholera infections.
Treatment:
Prompt treatment of cholera is essential to prevent complications and reduce the risk of mortality, particularly in severe cases. Oral rehydration therapy (ORT) is the cornerstone of cholera treatment and involves replenishing fluids and electrolytes lost through diarrhea and vomiting. ORT solutions, consisting of a precise balance of salts, sugars, and water, are administered orally or through nasogastric tubes to restore hydration and maintain electrolyte balance.
In severe cases of dehydration, intravenous fluids may be necessary to rapidly replace fluid losses and correct electrolyte imbalances. Antibiotics such as doxycycline or azithromycin may be prescribed to reduce the duration and severity of diarrhea and shorten the shedding of Vibrio cholerae bacteria. Zinc supplementation may also be recommended to support immune function and reduce the duration of diarrheal illness, particularly in children.
- Rehydration Therapy: The cornerstone of cholera treatment is rehydration therapy, aimed at restoring fluid and electrolyte balance in individuals affected by profuse diarrhea and vomiting. Oral rehydration solution (ORS), consisting of a precise combination of salts, sugars, and water, is administered to replace lost fluids and electrolytes. ORS is effective, affordable, and easily administered, making it a vital component of cholera treatment, particularly in resource-limited settings.
- Intravenous Fluids: In severe cases of cholera with significant dehydration or electrolyte imbalances, intravenous (IV) fluids may be necessary to rapidly replenish fluid losses and correct abnormalities. IV fluids help restore circulation, maintain blood pressure, and prevent complications such as shock and organ failure. Electrolyte solutions containing salts such as sodium, potassium, and chloride are carefully administered to restore electrolyte balance and prevent further complications.
- Antibiotic Therapy: Antibiotics are commonly used in conjunction with rehydration therapy to shorten the duration and severity of cholera symptoms and reduce the shedding of Vibrio cholerae bacteria. Antibiotics such as doxycycline, azithromycin, or ciprofloxacin are effective in treating cholera and can help control the spread of the disease during outbreaks. However, antibiotic resistance is a growing concern, highlighting the importance of judicious antibiotic use and adherence to treatment guidelines.
- Zinc Supplementation: Zinc supplementation may be recommended, particularly in children with cholera, to support immune function and reduce the duration and severity of diarrheal illness. Zinc plays a crucial role in regulating immune responses and intestinal function, making it a valuable adjunct to rehydration therapy in the management of cholera.
- Antiemetic Medications: Antiemetic medications may be prescribed to control vomiting and nausea associated with cholera, allowing individuals to tolerate oral rehydration therapy more effectively. Antiemetics such as ondansetron or metoclopramide help alleviate symptoms and improve patient comfort during treatment.
- Nutritional Support: Adequate nutrition is essential for promoting recovery and preventing malnutrition in individuals affected by diarrheal illness. Nutritional support may include feeding oral rehydration solutions fortified with additional nutrients, such as glucose or amino acids, to provide energy and support tissue repair. In severe cases, supplemental feeding through nasogastric tubes or intravenous nutrition may be necessary to meet caloric and nutrient requirements.
- Isolation and Infection Control: During diarrheal illness outbreaks, isolation of affected individuals and strict infection control measures are crucial to prevent further transmission of the disease. Infected individuals should be isolated to reduce the risk of contaminating food, water, and surfaces with Vibrio cholerae bacteria. Healthcare workers should adhere to strict hand hygiene practices, wear appropriate personal protective equipment, and implement measures to disinfect contaminated areas to minimize the spread of infection.
- Community-based Management: Community-based management of diarrheal illness involves empowering local communities and healthcare providers to detect, treat, and prevent cholera outbreaks at the grassroots level. Training community health workers to recognize cholera symptoms, administer oral rehydration therapy, and promote hygiene and sanitation practices can improve access to timely care and reduce mortality rates associated with cholera.
- Monitoring and Surveillance: Continuous monitoring and surveillance of diarrheal illness cases and outbreaks are essential for guiding public health interventions and ensuring timely response to emerging threats. Surveillance systems help track disease trends, identify high-risk areas, and monitor the effectiveness of control measures. Rapid reporting of suspected cases and laboratory confirmation of diarrheal illness outbreaks enable public health authorities to implement targeted interventions and prevent further spread of the disease.
- Long-term Prevention Strategies: Long-term prevention strategies for diarrheal illness focus on improving water and sanitation infrastructure, promoting hygiene and sanitation practices, and enhancing access to clean water and sanitation facilities in vulnerable communities. Investment in safe drinking water supplies, wastewater treatment systems, and community sanitation programs is essential for reducing the burden of diarrheal illness and other waterborne diseases in the long term. Additionally, vaccination against cholera can provide additional protection for individuals at risk of exposure, particularly during outbreaks or in endemic regions.
These comprehensive treatment approaches aim to alleviate symptoms, prevent complications, and reduce the transmission of diarrheal illness, ultimately saving lives and improving public health outcomes. Collaborative efforts between healthcare providers, public health authorities, communities, and international organizations are essential for effectively managing cholera and mitigating its impact on affected populations.
Prevention:
Preventing diarrheal illness outbreaks requires a multi-faceted approach addressing both individual and community-level factors. Access to safe drinking water and improved sanitation facilities is paramount in reducing the risk of diarrheal illness transmission. Boiling or treating water with chlorine or other disinfectants can effectively kill the Vibrio cholerae bacterium and prevent contamination.
Promoting good hygiene practices, such as handwashing with soap and water, proper food handling and preparation, and safe disposal of fecal waste, helps minimize the spread of cholera and other diarrheal diseases. Vaccination against diarrheal illness is available for individuals traveling to endemic regions or during outbreaks, providing additional protection against the disease. Additionally, early detection and rapid response to suspected cases, along with surveillance and monitoring of water and sanitation systems, are critical in containing cholera outbreaks and preventing further transmission.
Conclusion:
Cholera remains a significant global health concern, particularly in regions with poor water and sanitation infrastructure and during emergencies or humanitarian crises. Understanding the causes, symptoms, treatment, and prevention strategies for cholera is essential for healthcare providers, policymakers, and communities to effectively control the spread of the disease and mitigate its impact on public health. By implementing comprehensive prevention and control measures and addressing underlying social determinants of health, we can work towards a future free from the threat of cholera and ensure access to clean water and sanitation for all.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023