Chronic Pancreatitis
Introduction
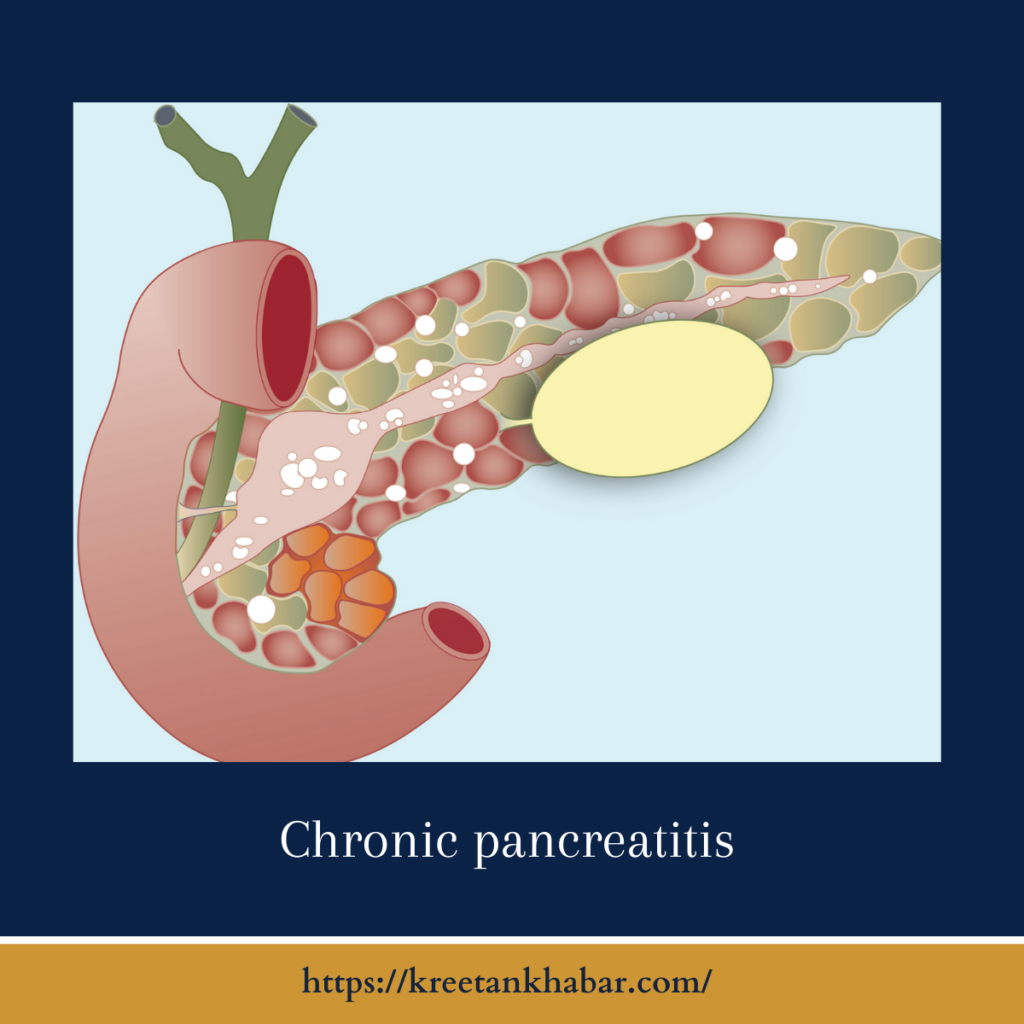
In the intricate landscape of gastrointestinal disorders, chronic pancreatitis stands as a painful and debilitating condition that affects countless individuals worldwide. Characterized by the persistent inflammation of the pancreas, this ailment can lead to a range of symptoms, from excruciating abdominal pain to malnutrition. In this article, we delve into the world of chronic pancreatitis, examining its causes, symptoms, diagnosis, and management.
Chronic Pancreatitis: A Pervasive Condition
Chronic pancreatitis is a long-term inflammation of the pancreas, an organ crucial for digestion and blood sugar regulation. Unlike acute pancreatitis, which is usually a sudden and severe condition, chronic pancreatitis develops gradually over time, causing irreversible damage to the pancreas.
Causes and Risk Factors
Several factors can contribute to the development of chronic pancreatitis, including:
- Alcohol Abuse: Chronic alcohol consumption is one of the leading causes of chronic pancreatitis. The toxic effects of alcohol can lead to pancreatic inflammation and scarring.
- Smoking: Cigarette smoking has been strongly linked to an increased risk of chronic pancreatitis.
- Genetic Factors: Some individuals may inherit genetic mutations that make them more susceptible to chronic pancreatitis.
- Obstruction: Blockages in the pancreatic ducts due to gallstones or other conditions can trigger inflammation.
- Autoimmune Disease: In rare cases, the body’s immune system may attack and damage the pancreas.
Symptoms and Complications
Chronic pancreatitis manifests with a range of distressing symptoms, which may include:
- Severe Abdominal Pain: The hallmark symptom of chronic pancreatitis is persistent and excruciating abdominal pain that often radiates to the back.
- Digestive Problems: The damaged pancreas may fail to produce sufficient digestive enzymes, leading to malabsorption, weight loss, and nutritional deficiencies.
- Diabetes: Chronic pancreatitis can disrupt insulin production, resulting in diabetes.
- Pancreatic Pseudocysts: Fluid-filled sacs can form in the pancreas, causing pain and potential complications.
here are key points outlining the symptoms and potential complications of chronic pancreatitis:
Symptoms:
- Persistent Abdominal Pain: The hallmark symptom of chronic pancreatitis is recurrent, severe abdominal pain that often radiates to the back.
- Digestive Problems: Malabsorption occurs as the damaged pancreas fails to produce sufficient digestive enzymes, leading to weight loss and nutritional deficiencies.
- Diarrhea: Frequent loose stools and diarrhea may result from impaired digestion and nutrient absorption.
- Nausea and Vomiting: Nausea and vomiting can be common, particularly after meals.
- Fatty Stool: Steatorrhea, or the presence of greasy, foul-smelling stools, indicates malabsorption of fats.
- Weight Loss: Ongoing malnutrition and reduced calorie absorption can lead to significant weight loss.
- Jaundice: If chronic pancreatitis causes blockages in the bile ducts, it may result in jaundice, characterized by yellowing of the skin and eyes.
- Chronic Pain Medications: The need for chronic pain management medications can lead to side effects and dependency.
Complications:
- Diabetes: Chronic pancreatitis can lead to impaired insulin production, causing diabetes mellitus.
- Pancreatic Pseudocysts: Fluid-filled sacs can form within or around the pancreas, potentially causing pain and infection.
- Pancreatic Insufficiency: As the pancreas deteriorates, it may lose its ability to produce essential digestive enzymes, further exacerbating malnutrition.
- Malnutrition: Inadequate nutrient absorption can result in malnutrition, leading to weakness and other health issues.
- Infection: Pseudocysts, pancreatic duct blockages, and impaired immune function increase the risk of pancreatic infections.
- Bowel Obstruction: Pancreatic pseudocysts can press on the intestines, causing bowel obstructions.
- Breathing Difficulties: Pressure on the diaphragm due to an enlarged pancreas or pseudocysts may lead to breathing difficulties.
- Blood Vessel Issues: Chronic inflammation can affect blood vessels, potentially causing thrombosis or bleeding.
- Pancreatic Cancer Risk: Individuals with chronic pancreatitis may have a slightly elevated risk of developing pancreatic cancer.
- Psychological Impact: Living with chronic pain and digestive issues can lead to depression, anxiety, and decreased quality of life.
Understanding the symptoms and potential complications of chronic pancreatitis is crucial for timely diagnosis and management. Early intervention and a comprehensive treatment plan can help improve the prognosis and quality of life for individuals facing this challenging condition.
Diagnosis and Management
Diagnosing chronic pancreatitis typically involves a combination of medical history, physical exams, blood tests, and imaging studies like CT scans or MRI. Endoscopic tests such as endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) may also be employed.
Management of chronic pancreatitis aims to alleviate symptoms and prevent complications:
- Pain Management: Pain relief is a primary concern, often requiring medications, lifestyle modifications, and, in severe cases, nerve block procedures.
- Nutritional Support: Enzyme replacement therapy and dietary changes can help patients manage malabsorption and malnutrition.
- Diabetes Control: Diabetes management becomes essential if it develops as a result of chronic pancreatitis.
- Lifestyle Changes: Avoiding alcohol and smoking, along with maintaining a healthy diet, is crucial to managing the condition.
- Surgery: In severe cases, surgery may be necessary to remove damaged pancreatic tissue or manage complications like pseudocysts.
here are key points regarding the diagnosis and management of chronic pancreatitis:
Diagnosis:
- Clinical Evaluation: Diagnosis begins with a thorough medical history, physical examination, and evaluation of symptoms, particularly persistent abdominal pain.
- Blood Tests: Blood tests may reveal elevated levels of pancreatic enzymes, such as amylase and lipase, but normal levels do not rule out chronic pancreatitis.
- Imaging Studies: CT scans, MRIs, and ultrasound can visualize the pancreas and detect structural changes or pseudocysts.
- Endoscopic Tests: Endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) provide detailed images of the pancreas and its ducts.
- Stool Tests: Stool tests may indicate malabsorption and fat excretion due to insufficient digestive enzymes.
Management:
- Pain Control: Pain management is a primary focus, involving medications, lifestyle adjustments, and interventions like nerve blocks for severe pain.
- Nutritional Support: Enzyme replacement therapy (ERT) helps patients digest food and absorb nutrients properly, addressing malabsorption and malnutrition.
- Dietary Modifications: A low-fat diet, small frequent meals, and avoidance of alcohol and spicy foods can help manage symptoms.
- Diabetes Management: If diabetes develops due to impaired insulin production, proper blood sugar control is essential.
- Smoking and Alcohol Cessation: Avoiding smoking and alcohol is crucial to prevent further pancreatic damage.
- Surgery: Surgery may be necessary for complications like pseudocysts or in cases of severe pain unresponsive to other treatments.
- Pancreatic Enzyme Replacement: Pancreatic enzyme supplements are essential to compensate for enzyme deficiencies and improve digestion.
- Lifestyle Changes: Maintaining a healthy lifestyle, including regular exercise and weight management, can help manage symptoms.
- Psychological Support: Living with chronic pancreatitis can be mentally challenging; seeking psychological support or counseling can be beneficial.
- Regular Follow-Up: Patients with chronic pancreatitis require regular check-ups and monitoring to assess disease progression and adjust treatment as needed.
In summary, the diagnosis and management of chronic pancreatitis involve a multifaceted approach, addressing pain, digestive issues, and complications while emphasizing lifestyle modifications and ongoing medical care. Early intervention and a tailored treatment plan can significantly improve the quality of life for individuals living with this condition.
Conclusion
Chronic pancreatitis is a challenging condition that significantly impacts the lives of those affected. Early diagnosis and comprehensive management are key to improving the quality of life for individuals living with this ailment. By understanding the causes, symptoms, and available treatment options, both patients and healthcare providers can work together to mitigate the struggles associated with chronic pancreatitis and offer hope for a better tomorrow.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023