Chronic Venous Insufficiency: A Comprehensive Guide to Causes, Symptoms, and Management
Introduction:
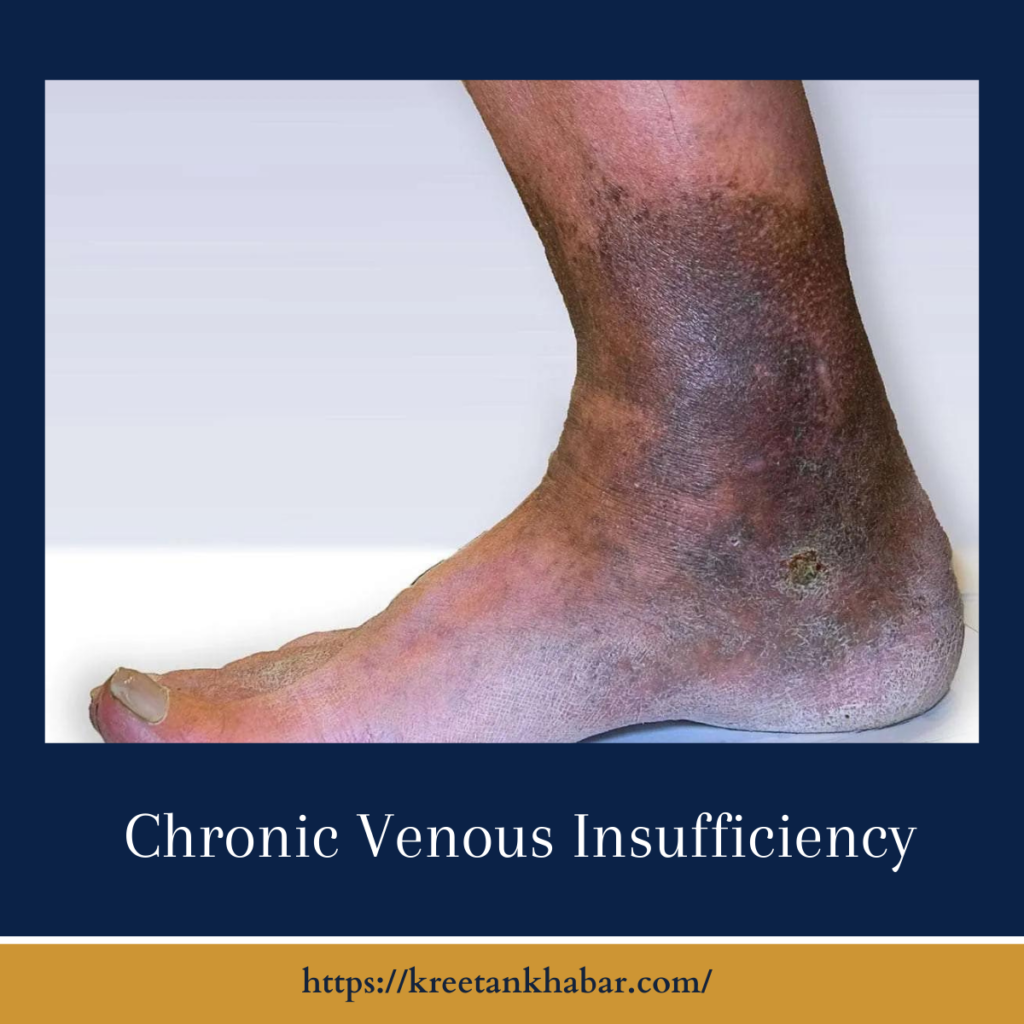
Chronic Venous Insufficiency (CVI) is a vascular condition that often lingers in the shadows, affecting the veins in the legs and causing a cascade of symptoms that impact daily life. In this comprehensive guide, we aim to shed light on the complexities of Chronic Venous Insufficiency, exploring its root causes, manifestations, diagnostic approaches, and the diverse array of management strategies available to those navigating this condition.
Understanding Chronic Venous Insufficiency:
Chronic Venous Insufficiency is a condition characterized by the impaired function of the valves within the leg veins, compromising the efficient return of blood to the heart. This insufficiency leads to a pooling of blood in the lower extremities, giving rise to various symptoms and potential complications.
Causes of Chronic Venous Insufficiency:
- Venous Valve Dysfunction: The primary culprit behind CVI is the malfunction of valves within the veins. These valves, crucial for maintaining unidirectional blood flow, may become weakened or damaged, allowing blood to flow backward and accumulate in the veins.
- Deep Vein Thrombosis (DVT): A history of deep vein thrombosis, wherein blood clots form in the deep veins, can result in valve damage, contributing to the development of CVI.
- Varicose Veins: Enlarged and twisted veins near the skin’s surface, known as varicose veins, can compromise the integrity of vein valves and serve as a precursor to Chronic Venous Insufficiency.
- Pregnancy: The increased blood volume and pressure during pregnancy can strain pelvic veins, potentially leading to valve weakening and the subsequent onset of CVI.
- Obesity: Excess weight puts additional pressure on veins, increasing the risk of valve damage and contributing to the development of Chronic Venous Insufficiency.
- Aging: The natural aging process can lead to wear and tear on vein valves, diminishing their effectiveness and elevating the susceptibility to CVI.
Symptoms of Chronic Venous Insufficiency:
- Leg Pain and Aching: Individuals with CVI often experience persistent pain or aching sensations in the legs, particularly after prolonged periods of standing or sitting.
- Swelling: Edema or swelling in the legs and ankles is a hallmark symptom of Chronic Venous Insufficiency, resulting from compromised blood flow.
- Skin Changes: Changes in skin color, including discoloration or darkening, may occur in the affected areas. Additionally, the skin may become dry, itchy, or exhibit a leathery texture.
- Varicose Veins: The presence of visible varicose veins is a common indicator of venous insufficiency, reflecting compromised valve function.
- Leg Ulcers: In advanced stages, CVI can lead to the development of venous ulcers, particularly in the lower leg. These ulcers may be slow to heal and prone to infection.
Diagnosis of Chronic Venous Insufficiency:
- Clinical Evaluation: A thorough physical examination, including a review of medical history and an assessment of symptoms, forms the initial diagnostic approach.
- Doppler Ultrasound: This non-invasive imaging test utilizes sound waves to evaluate blood flow and detect abnormalities in the veins. Doppler ultrasound is instrumental in assessing venous insufficiency.
- Venous Reflux Exam: Specialized tests measure backward blood flow in the veins, aiding in the identification of valve dysfunction and the extent of CVI.
- CT or MRI Venography: In certain cases, advanced imaging studies provide detailed images of the veins, helping identify any blockages or abnormalities.
The points of diagnosis:
Management of Chronic Venous Insufficiency:
- Compression Therapy: Wearing compression stockings applies external pressure, reducing swelling and improving blood flow in the legs.
- Lifestyle Modifications: Encouraging patients to elevate their legs, engage in regular exercise, and avoid prolonged periods of sitting or standing helps manage symptoms and enhances blood circulation.
- Medications: Diuretics may be prescribed to reduce swelling, while anti-inflammatory drugs can alleviate pain and discomfort associated with CVI.
- Endovenous Ablation: A minimally invasive procedure, endovenous ablation employs heat or laser energy to close malfunctioning veins, redirecting blood flow to healthier vessels.
- Sclerotherapy: Injecting a solution into varicose veins causes them to collapse and fade, offering a non-surgical approach to treat smaller veins.
- Vein Stripping: In severe cases, surgical intervention may be necessary to remove or tie off damaged veins, allowing blood to reroute through healthier vessels.
- Laser Therapy: Laser treatment targets and closes varicose veins, alleviating symptoms and improving the appearance of affected areas.
Conclusion:
Chronic Venous Insufficiency, though often underestimated, can significantly impact an individual’s quality of life. Early recognition of symptoms, coupled with a personalized treatment plan that may involve lifestyle adjustments, medications, or various procedures, is crucial for effective management. By understanding the intricacies of CVI and exploring diverse therapeutic avenues, those affected can take proactive steps toward regaining control and embracing a healthier, more comfortable life.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023