Cushing Disease: Unmasking the Impact of Excess Cortisol
Cushing Disease(also known as hypercortisolism) is a rare and complex medical condition that affects the endocrine system, causing the overproduction of cortisol, a vital hormone in the body. While the name may not be as familiar as other health issues, the consequences of this disease can be severe. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for Cushing’s Disease.
Understanding Cushing’s Disease:
hypercortisolism is a subset of a broader condition known as Cushing’s Syndrome, which can result from various causes, including the prolonged use of corticosteroid medications. However, Cushing’s Disease specifically originates in the pituitary gland. The pituitary gland, located at the base of the brain, produces adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands to release cortisol, a hormone that plays a crucial role in regulating metabolism, immune function, and the body’s response to stress.
Causes of Cushing’s Disease:
Cushing’s Disease is primarily caused by the presence of a noncancerous tumor, known as an adenoma, in the pituitary gland. This adenoma releases excessive amounts of ACTH, which, in turn, signals the adrenal glands to produce more cortisol than the body needs. Less commonly, hypercortisolism can result from tumors in the lungs or other tissues that produce ACTH.
Symptoms of Cushing’s Disease:
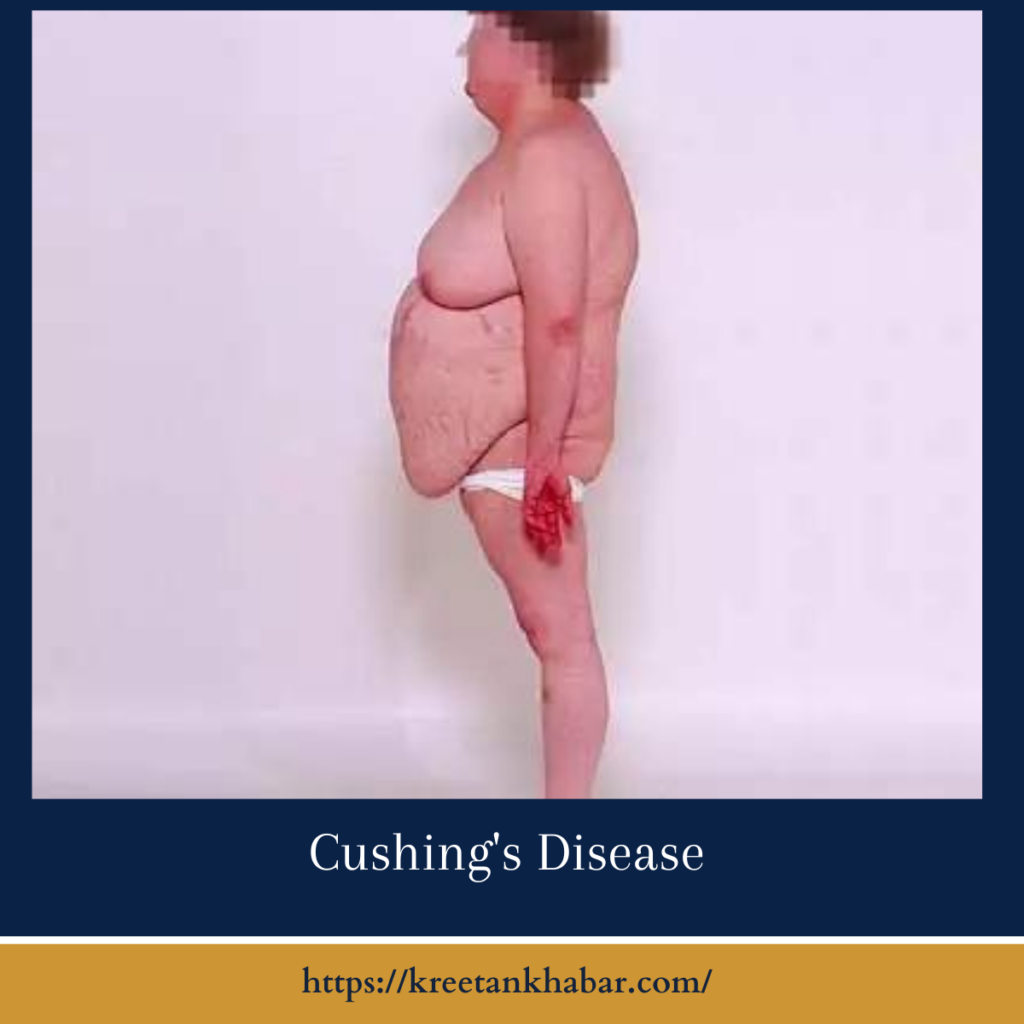
The signs and symptoms of hypercortisolism can vary from person to person, and their onset is often gradual. Common indicators include:
- Weight Gain: Patients may experience unexplained weight gain, particularly in the abdominal area, face, and upper back (referred to as a “moon face” and “buffalo hump”).
- High Blood Pressure: Elevated blood pressure is a frequent consequence of excess cortisol.
- Muscle Weakness: Muscle atrophy and weakness can lead to difficulties in physical activities.
- Skin Changes: Patients may notice changes in the skin, such as thinning, bruising, and the development of purple stretch marks.
- Glucose Intolerance: Cortisol interferes with insulin’s action, leading to elevated blood sugar levels and an increased risk of diabetes.
- Mood Disturbances: Emotional disturbances like depression, anxiety, and irritability can be a part of hypercortisolism.
- Osteoporosis: Weakened bones are a concern due to the loss of calcium from bones into the bloodstream.
- Menstrual Irregularities: In women, hypercortisolism can lead to irregular menstrual cycles.
- Reduced Libido and Erectile Dysfunction: Men may experience sexual difficulties.
Diagnosis of Cushing’s Disease:
Diagnosing Cushing’s Disease can be challenging, given its gradual onset and the variability of symptoms. The diagnostic process typically includes:
- Hormone Tests: Blood and urine tests are performed to measure cortisol levels. A 24-hour urinary free cortisol test is commonly used.
- Dexamethasone Suppression Test: This test assesses how the body responds to dexamethasone, a synthetic cortisol. Failure to suppress cortisol production is indicative of hypercortisolism.
- Imaging: Imaging studies, such as MRI or CT scans, are used to identify tumors in the pituitary gland or elsewhere.
- ACTH Blood Test: Measuring the level of ACTH can help determine whether the source of excess cortisol is pituitary-based (as in Cushing’s Disease) or from an external tumor.
Diagnosis of Cushing’s Disease: A Comprehensive Guide
- Clinical Evaluation: The diagnostic process typically begins with a comprehensive clinical evaluation by a healthcare provider. The medical history is reviewed, and any presenting symptoms or signs that may suggest Cushing’s Disease are assessed.
- Symptom Assessment: Symptoms that raise suspicion of Cushing Disease include unexplained weight gain, particularly in the face and upper back, muscle weakness, skin changes, high blood pressure, and mood disturbances.
- Hormone Tests: Measuring cortisol levels through blood and urine tests is a fundamental step. The 24-hour urinary free cortisol test is commonly used to determine the amount of cortisol excreted in urine over a day.
- Midnight Salivary Cortisol Test: Salivary cortisol levels may be measured at midnight, as they should typically be lower at this time. Elevated levels may suggest Cushing Disease.
- Dexamethasone Suppression Test: This test assesses how the body responds to dexamethasone, a synthetic cortisol. Patients take dexamethasone, and cortisol levels are measured. A lack of cortisol suppression indicates Cushing’s Disease.
- Late-Night Salivary Cortisol Test: Similar to the midnight salivary cortisol test, this test measures cortisol levels in saliva late at night to evaluate its circadian rhythm.
- Low-Dose Dexamethasone Suppression Test: This test involves taking a low dose of dexamethasone and measuring cortisol levels the next day. Lack of suppression suggests Cushing Disease.
- High-Dose Dexamethasone Suppression Test: In this test, high doses of dexamethasone are administered, and cortisol levels are checked. It can help distinguish between pituitary and non-pituitary causes of excess cortisol.
- ACTH Measurement: Measuring the levels of adrenocorticotropic hormone (ACTH) in the blood helps differentiate between pituitary-dependent Cushing Disease and other causes.
- Imaging Studies: Radiological imaging, such as MRI or CT scans, is employed to visualize the pituitary gland and identify any tumors or abnormalities.
- Bilateral Inferior Petrosal Sinus Sampling (BIPSS): In complex cases, BIPSS may be performed to distinguish between pituitary and non-pituitary sources of ACTH production.
- ACTH Stimulation Test: In cases where the source of excess cortisol is not clear, an ACTH stimulation test may be used to provoke cortisol release and help pinpoint the issue.
- Genetic Testing: Genetic testing is considered in rare cases where a genetic predisposition to Cushing Disease is suspected.
- Confirmation: A definitive diagnosis of Cushing Disease is typically made when the healthcare provider confirms elevated cortisol levels and identifies the source of excess cortisol, often a pituitary adenoma.
In conclusion, the diagnosis of Cushing Disease is a multifaceted process that involves a combination of clinical evaluation, hormone testing, and imaging studies. Accurate diagnosis is crucial for effective management and treatment of this condition. If Cushing Disease is suspected, seeking the expertise of an endocrinologist and undergoing the necessary diagnostic tests is essential to confirm the diagnosis and initiate appropriate care.
Treatment Options for Cushing’s Disease:
The goal of treatment for Cushing Disease is to normalize cortisol levels and address the underlying cause. Treatment options include:
- Surgery: Transsphenoidal surgery is often recommended to remove pituitary tumors responsible for Cushing Disease. When the tumor cannot be entirely removed, radiation therapy may be considered.
- Medications: In cases where surgery is not an option or does not fully resolve the condition, medications like ketoconazole, mifepristone, and pasireotide can be used to control cortisol production.
- Lifestyle Changes: Patients are advised to manage their diet, exercise, and stress levels to support overall health and maintain cortisol balance.
Conclusion
Cushing’s Disease, though rare, can have a significant impact on a person’s health and quality of life. Early diagnosis and appropriate treatment are essential to prevent complications and help individuals regain hormonal balance. If you suspect Cushing Disease due to the presence of its symptoms, seeking medical attention and consultation with an endocrinologist is the first step towards effective management and improved well-being.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023