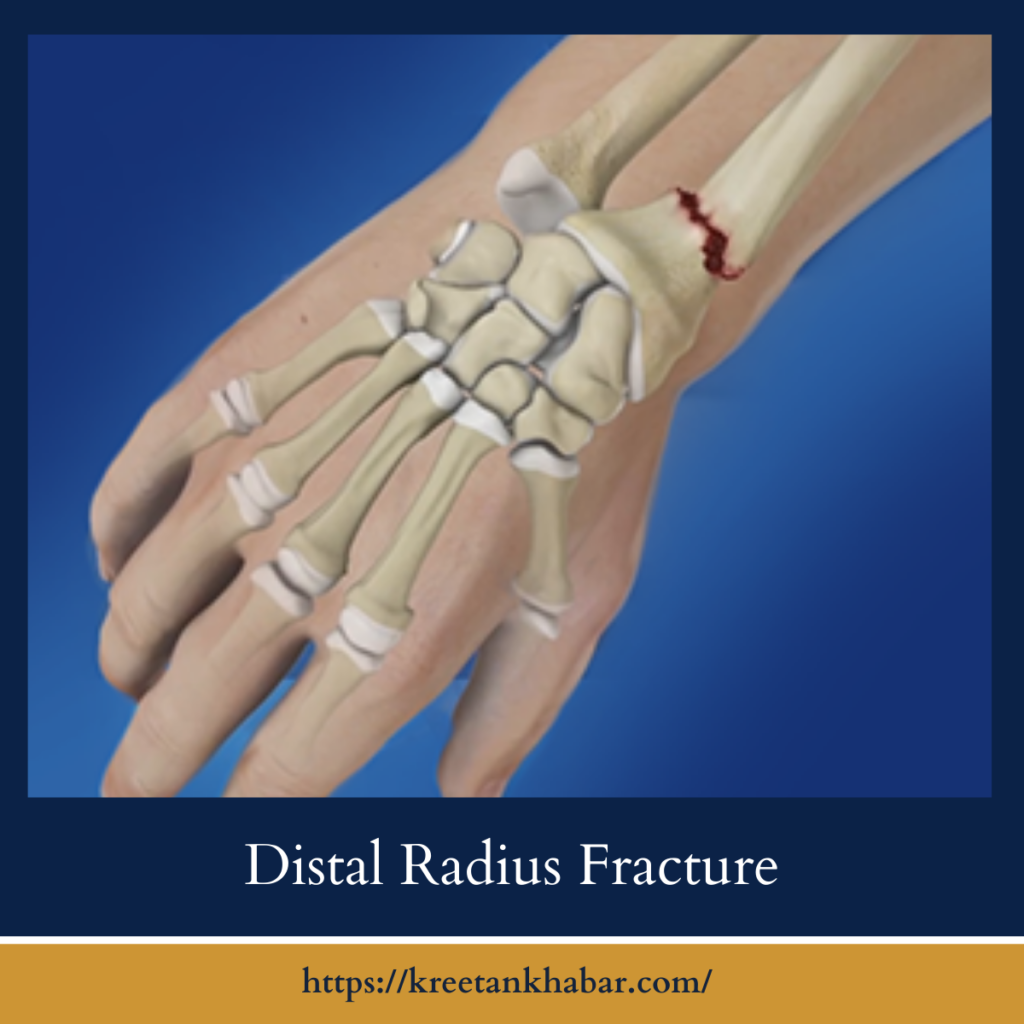
Distal Radius Fracture: Causes, Symptoms, and Recovery
A distal radius fracture, commonly known as a broken wrist, is a prevalent injury that can significantly impact daily life. Whether resulting from a fall, sports mishap, or accident, understanding the causes, symptoms, and recovery process is essential for managing this orthopedic condition effectively. In this article, we delve into the intricacies of a distal radius fracture, providing insights into its diagnosis, treatment options, and tips for a smooth recovery journey.
Understanding the Injury
A distal radius fracture occurs when the radius bone in the forearm breaks near the wrist joint. The radius is one of the two bones in the forearm, and its distal end, near the wrist, is particularly vulnerable to fractures due to the force exerted during falls or impacts. Depending on the severity and location of the fracture, treatment approaches may vary, ranging from conservative measures to surgical intervention.
Causes and Risk Factors
Distal radius fractures often result from trauma or excessive force applied to the wrist joint. Common causes include falls onto an outstretched hand, direct blows to the wrist, or sudden impacts during sports activities. Individuals at higher risk for distal radius fractures include older adults, who may experience decreased bone density and increased susceptibility to fractures, as well as athletes participating in high-impact sports or activities.
- Falls onto an Outstretched Hand: One of the most common causes of a distal radius fracture is a fall onto an outstretched hand. When an individual falls, instinctively extending their hand to break the fall, the force exerted on the wrist can lead to a fracture of the distal end of the radius bone.
- Sports Injuries: Participation in sports activities, particularly those involving high impact or contact, increases the risk of sustaining a distal radius fracture. Sports such as skateboarding, snowboarding, skiing, and basketball pose a higher risk due to the potential for falls or collisions that can result in wrist injuries.
- Accidental Trauma: Accidents involving direct blows or trauma to the wrist, such as motor vehicle accidents, workplace injuries, or slips and trips, can cause fractures in the distal radius. The force of impact can exceed the strength of the bone, leading to a fracture.
- Osteoporosis: Individuals with osteoporosis, a condition characterized by low bone density and increased bone fragility, are at higher risk of sustaining a distal radius fracture. Weakened bones are more susceptible to fractures from minor trauma or falls, making individuals with osteoporosis particularly vulnerable.
- Aging: Age-related changes in bone density and strength increase the risk of distal radius fractures, especially among older adults. As people age, bone density decreases, and bones become more brittle, making them more prone to fractures from even minor trauma or falls.
- Gender: Studies have shown that women are more likely than men to sustain distal radius fractures, particularly after menopause. The decline in estrogen levels during menopause contributes to decreased bone density and increased susceptibility to fractures in women.
- Previous Fractures: Individuals who have previously experienced a distal radius fracture or other wrist injuries are at higher risk of sustaining another fracture. Prior injuries may weaken the bone or alter the biomechanics of the wrist, increasing the likelihood of future fractures.
- Genetic Factors: Genetic predisposition may play a role in determining an individual’s susceptibility to distal radius fractures. Family history of osteoporosis or a tendency to have weaker bones may increase the risk of fractures, including distal radius fractures, among family members.
- Certain Medications: Long-term use of certain medications, such as corticosteroids or anticonvulsants, can weaken bones and increase the risk of fractures, including distal radius fractures. These medications may affect bone density and bone metabolism, leading to increased bone fragility.
- Lifestyle Factors: Lifestyle choices such as smoking, excessive alcohol consumption, and poor nutrition can weaken bones and increase the risk of fractures, including distal radius fractures. Smoking, in particular, has been linked to decreased bone density and impaired bone healing, making smokers more susceptible to fractures.
Understanding the various causes and risk factors associated with a distal radius fracture can help individuals take preventive measures, make informed lifestyle choices, and seek appropriate medical care to reduce their risk of injury and promote bone health.
Symptoms
The symptoms of a distal radius fracture can vary depending on the severity and type of fracture. Common signs and symptoms may include:
- Pain: Persistent pain in the wrist, which may worsen with movement or pressure.
- Swelling: Swelling and tenderness around the wrist joint, accompanied by bruising or discoloration.
- Limited Range of Motion: Difficulty moving the wrist or performing daily activities due to pain and stiffness.
- Visible Deformity: In severe cases, a visible deformity or misalignment of the wrist bones may be present.
- Numbness or Tingling: Numbness, tingling, or weakness in the hand or fingers, indicating nerve involvement.
Diagnosis and Treatment
Diagnosis of a distal radius fracture typically involves a physical examination, evaluation of symptoms, and imaging tests such as X-rays or CT scans to assess the extent of the injury. Treatment options vary depending on factors such as the severity and displacement of the fracture, as well as the individual’s age and activity level. Treatment may include:
- Immobilization: For minor fractures, wearing a splint or cast may be sufficient to immobilize the wrist and promote healing.
- Reduction: In cases of displaced fractures, a procedure called closed reduction may be performed to realign the bones manually.
- Surgery: Severe or complex fractures may require surgical intervention, such as open reduction and internal fixation (ORIF), to stabilize the bones with screws, plates, or pins.
- Rehabilitation: Following immobilization or surgery, physical therapy and rehabilitation exercises are essential to restore strength, flexibility, and function to the wrist joint.
Recovery and Rehabilitation
The recovery period for a distal radius fracture varies depending on factors such as the severity of the injury, the type of treatment received, and the individual’s overall health. During the initial phase of healing, rest, elevation, and icing can help reduce pain and swelling. As symptoms improve, gradual rehabilitation exercises prescribed by a physical therapist can promote recovery and prevent stiffness.
Coping Strategies and Support
Coping with a distal radius fracture can be challenging, both physically and emotionally. It’s essential to prioritize self-care, follow medical advice, and seek support from friends, family, or support groups if needed. Simple modifications to daily activities, such as using assistive devices or adapting work tasks, can help facilitate recovery and maintain independence during the healing process.
In conclusion,
a distal radius fracture is a common orthopedic injury that requires prompt diagnosis, appropriate treatment, and careful rehabilitation for optimal outcomes. By understanding the causes, symptoms, and treatment options associated with a distal radius fracture, individuals can take proactive steps to manage their injury effectively and regain function in the wrist joint. With patience, perseverance, and support from healthcare professionals, family, and friends, most people can recover fully from a distal radius fracture and resume their normal activities with time.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023