Donovanosis: Unraveling the Enigmatic World of Granuloma Inguinale
Introduction:
In the realm of sexually transmitted infections, Donovanosis(also known as venereal granuloma) stands as a lesser-known yet intriguing entity. Also known as granuloma inguinale, this bacterial infection is caused by Klebsiella granulomatis and primarily affects the genital and perianal regions. venereal granuloma might not be as prevalent as some other sexually transmitted diseases, but its unique characteristics make it a topic worth exploring. In this article, we delve into the enigmatic world of venereal granuloma, examining its etiology, clinical features, diagnosis, and the challenges surrounding its management.
Etiology:
- Klebsiella Granulomatis:
- Donovanosis is caused by the bacterium Klebsiella granulomatis. This gram-negative bacillus is responsible for the development of characteristic lesions in the genital and perianal regions.
Clinical Features:
- Painless Ulcerative Lesions:
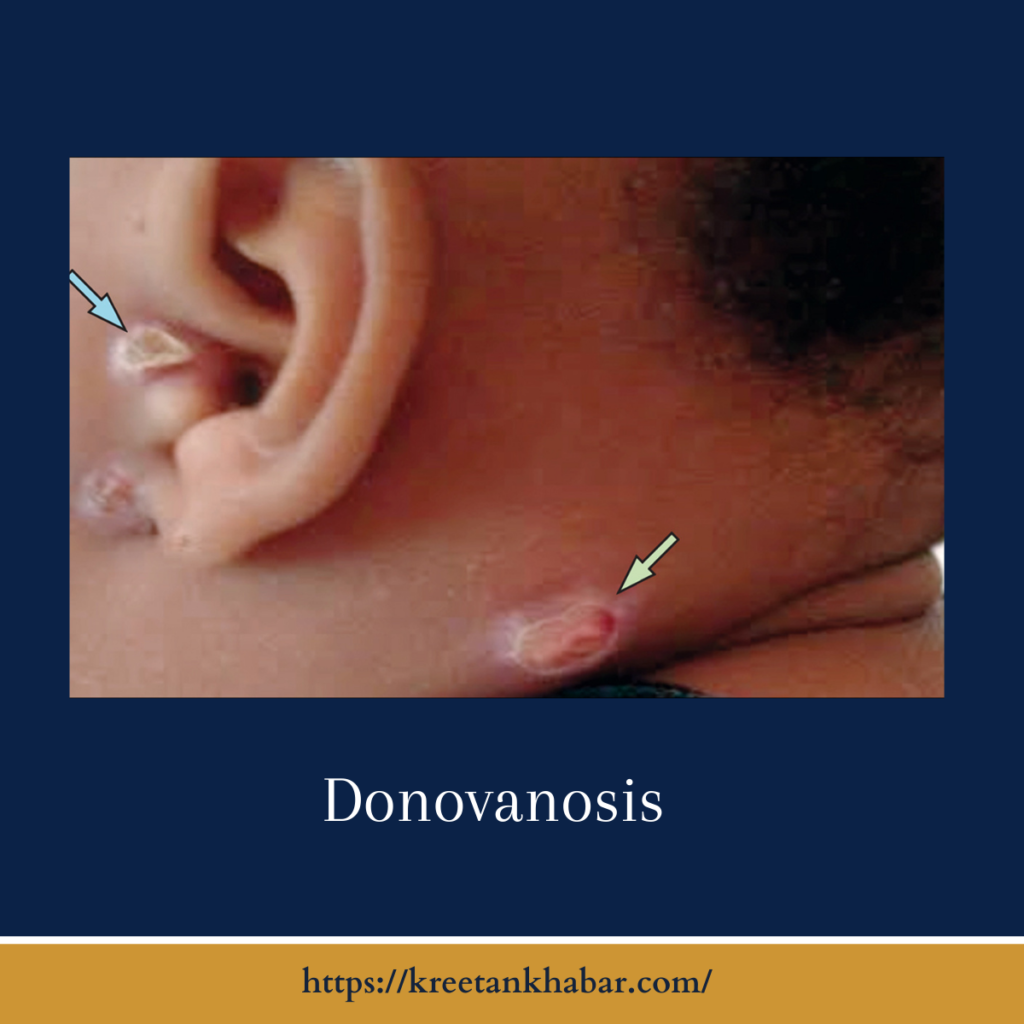
- One of the distinct features of venereal granuloma is the development of painless, beefy-red, ulcerative lesions. These lesions can be mistaken for other genital ulcers, adding to the diagnostic challenges.
- Slow Progression:
- Donovanosis is known for its slow progression. The ulcerative lesions may enlarge over time and can extend into surrounding tissues if left untreated.
- Regional Lymph Node Involvement:
-
- In advanced cases, venereal granuloma can involve regional lymph nodes, leading to the formation of granulomatous masses known as “groove sign.”
Diagnosis:
Diagnosing Donovanosis, also known as granuloma inguinale, is a nuanced process that involves a combination of clinical evaluation and laboratory testing. The distinctive feature of painless ulcerative lesions in the genital and perianal regions is a crucial clinical clue. However, due to the similarity of these lesions to other genital ulcers, a definitive diagnosis often requires confirmatory laboratory testing.
Microscopic examination of tissue samples obtained from the lesions is a key diagnostic approach. The identification of Donovan bodies, which are encapsulated bacteria within macrophages, is a hallmark sign of the infection. This microscopic confirmation is essential for ruling out other genital ulcers and ensuring accurate and timely treatment. The diagnostic journey of venereal granuloma underscores the importance of a comprehensive approach, combining clinical acumen with precise laboratory analysis to guide effective management strategies.
- Clinical Presentation:
- Diagnosis often relies on the clinical presentation of ulcerative lesions, which may exhibit characteristic features. However, the similarity to other genital ulcers necessitates confirmatory laboratory testing.
- Microscopic Examination:
-
- Microscopic examination of tissue samples obtained from the lesions is a crucial diagnostic tool. The identification of Donovan bodies, encapsulated bacteria within macrophages, is indicative of the infection.
Points of diagnosis:
- Clinical Evaluation:
- Initiate the diagnostic process through clinical evaluation, considering the presence of painless ulcerative lesions in the genital and perianal regions, which are characteristic of venereal granuloma.
- Laboratory Testing:
- Confirmatory laboratory testing is essential due to the similarity of venereal granuloma lesions to other genital ulcers. Microscopic examination of tissue samples obtained from the lesions is a key diagnostic tool.
- Identification of Donovan Bodies:
- Microscopic examination aims to identify Donovan bodies, encapsulated bacteria within macrophages. The presence of these structures is a hallmark sign of venereal granuloma, distinguishing it from other genital ulcerations.
- Differential Diagnosis:
- Recognize the importance of a differential diagnosis, considering other sexually transmitted infections with similar clinical presentations. Laboratory testing helps rule out alternative causes of genital ulcers.
- Tissue Biopsy:
- In cases where clinical and microscopic findings are inconclusive, a tissue biopsy may be performed to obtain a more comprehensive understanding and confirm the presence of Donovanosis.
- PCR Testing:
- Polymerase Chain Reaction (PCR) testing may be employed for its sensitivity in detecting the genetic material of Klebsiella granulomatis, providing additional confirmation of venereal granuloma.
- Collaboration with Pathologists:
- Collaborate with pathologists to ensure accurate interpretation of microscopic findings, fostering a multidisciplinary approach for a precise and timely diagnosis.
- Timely Diagnosis:
- Emphasize the importance of timely diagnosis to initiate appropriate treatment promptly, preventing the progression of venereal granuloma and potential complications.
- Clinical Acumen:
- Acknowledge the significance of clinical acumen in recognizing the unique characteristics of venereal granuloma lesions, prompting healthcare providers to consider this rare bacterial infection in their differential diagnosis.
- Communication with Patients:
- Communicate effectively with patients, explaining the diagnostic process, and addressing any concerns or questions they may have about venereal granuloma, fostering a collaborative and informed approach to healthcare.
Management Challenges:
- Limited Treatment Options:
- Donovanosis poses challenges in management due to limited treatment options. Antibiotics like azithromycin and doxycycline are commonly used, but resistance can complicate the therapeutic landscape.
- Potential for Complications:
-
- If left untreated, venereal granuloma can lead to severe tissue destruction and scarring. The potential for complications underscores the importance of early and effective intervention.
Prevention and Public Health:
Preventing Donovanosis is intricately tied to practicing safe sex and fostering robust public health initiatives. Given its relatively low prevalence, raising awareness about venereal granuloma is crucial to educating individuals about the risks and transmission modes of this bacterial infection. Safe sexual practices, including the consistent use of barrier methods like condoms, play a pivotal role in preventing its spread.
Public health efforts should focus on enhanced surveillance to monitor and understand the epidemiology of venereal granuloma, informing targeted interventions and preventive strategies. Education campaigns, both within healthcare settings and the broader community, can contribute to early recognition of symptoms, prompt diagnosis, and timely treatment. By integrating preventive measures into public health agendas and promoting safe sexual behaviors, we can collectively work towards reducing the incidence of Donovanosis and ensuring the well-being of individuals and communities.
- Safe Sexual Practices:
- Preventing Donovanosis involves practicing safe sex, including the consistent use of barrier methods such as condoms. Educating individuals about the risks and transmission of the infection is vital.
- Enhanced Surveillance:
-
- Due to its relatively low prevalence, Donovanosis benefits from enhanced surveillance efforts to monitor and understand its epidemiology. This can inform public health strategies for prevention and control.
Points of pevention and public health:
- Safe Sexual Practices:
- Emphasize the importance of consistent and correct condom use during sexual activities to reduce the risk of Donovanosis transmission.
- Education Campaigns:
- Implement educational initiatives to increase awareness about Donovanosis, focusing on its clinical features, modes of transmission, and the significance of early detection.
- Regular STI Screenings:
- Encourage individuals to undergo regular sexually transmitted infection (STI) screenings, especially those engaged in high-risk behaviors, to facilitate early diagnosis and intervention.
- Healthcare Provider Training:
- Provide training for healthcare providers to enhance their understanding of Donovanosis, ensuring accurate diagnosis and effective communication of preventive measures to patients.
- Enhanced Surveillance:
- Implement enhanced surveillance systems to monitor the prevalence and distribution of Donovanosis, enabling a more targeted and proactive public health response.
- Community Outreach:
- Engage in community outreach programs to disseminate information about Donovanosis, addressing misconceptions and promoting a proactive approach to sexual health.
- Partner Notification Programs:
- Develop partner notification programs to encourage individuals diagnosed with Donovanosis to inform their sexual partners, facilitating prompt testing and preventive measures.
- Integration with STI Prevention Efforts:
- Integrate Donovanosis prevention into broader STI prevention efforts, recognizing its unique characteristics and risk factors to tailor interventions effectively.
- Accessible Testing and Treatment Services:
- Ensure accessibility to testing and treatment services for Donovanosis, removing barriers that may hinder individuals from seeking timely healthcare.
- Research and Development:
- Invest in research and development to explore preventive strategies, potential vaccines, and innovative approaches to further strengthen the public health response to Donovanosis.
Conclusion:
While Donovanosis might linger in the shadows of more widely discussed sexually transmitted infections, its unique clinical presentation and diagnostic challenges make it an intriguing subject for both healthcare professionals and the general public. As we navigate the complexities of sexually transmitted diseases, shedding light on lesser-known entities like Donovanosis becomes imperative for comprehensive awareness and effective public health strategies.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023