Eosinophilic Fasciitis: Understanding a Rare Connective Tissue Disorder
Introduction
Eosinophilic Fasciitis (EF), a rare and poorly understood connective tissue disorder, is characterized by inflammation and thickening of the fascia, the connective tissue that surrounds muscles, tendons, and ligaments. This condition can lead to pain, swelling, and skin changes, often affecting the extremities. In this article, we will delve into the complexities of eosinophilic fasciitis, including its causes, symptoms, diagnosis, and treatment options.
Understanding Eosinophilic Fasciitis
Eosinophilic Fasciitis, also known as Shulman’s Syndrome, is a rare autoimmune disorder that primarily affects adults, with a higher prevalence in men. It is characterized by inflammation and thickening of the fascia, leading to functional limitations and discomfort. Although the exact cause remains unclear, EF is believed to involve autoimmune processes.
Causes of Eosinophilic Fasciitis
The precise cause of eosinophilic fasciitis is not well-defined. However, several factors are thought to contribute to the development of this condition:
- Autoimmune Dysfunction: EF is considered an autoimmune disorder, where the immune system mistakenly attacks the body’s own tissues, resulting in inflammation and damage to the fascia.
- Infection and Environmental Triggers: Some cases of EF may be triggered by viral or bacterial infections, as well as environmental factors, although these links are not fully established.
Symptoms and Manifestations
Eosinophilic Fasciitis can present with a variety of symptoms, which may include:
- Pain and Stiffness: Pain and stiffness in the affected limbs are common early symptoms. This discomfort can limit joint movement and function.
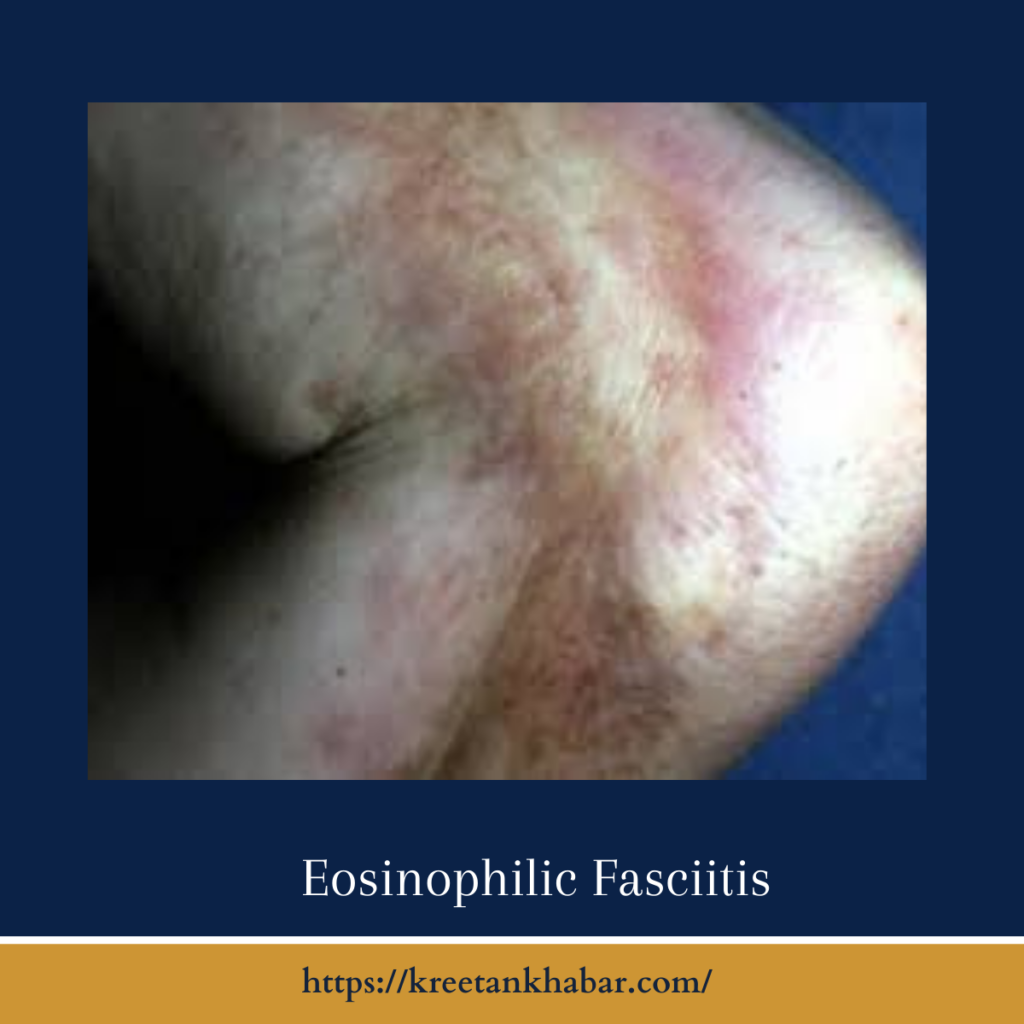
- Swelling and Skin Changes: Swelling of the limbs and changes in skin texture may occur, leading to skin thickening and a peau d’orange (orange peel) appearance.
- Eosinophilia: A characteristic feature of EF is an elevated eosinophil count in the blood. Eosinophils are a type of white blood cell involved in immune responses.
- Muscle Weakness: In some cases, muscle weakness may develop, further impairing the affected individual’s mobility.
- Symmetrical Involvement: EF often affects both sides of the body symmetrically, with a predilection for the arms and legs.
- Contractures: In advanced cases, the inflammation and thickening of the fascia can lead to contractures, which are permanent, fixed joint deformities.
here are key points about the symptoms and manifestations of Eosinophilic Fasciitis (EF):
1. Pain and Stiffness:
- The hallmark symptom of EF is pain and stiffness in the affected limbs, particularly the arms and legs.
- This discomfort can make it challenging to move the joints and can significantly limit mobility.
2. Swelling and Skin Changes:
- Swelling of the affected limbs is common in EF, often associated with a thickened appearance of the skin.
- The skin may take on a “peau d’orange” or “orange peel” texture due to the thickening.
3. Eosinophilia:
- A characteristic feature of EF is elevated levels of eosinophils in the blood.
- Eosinophils are a type of white blood cell involved in immune responses.
4. Muscle Weakness:
- In some cases, individuals with EF may experience muscle weakness, which can further impair movement and functionality.
5. Symmetrical Involvement:
- EF often affects both sides of the body symmetrically. For example, if one arm is affected, the other arm is likely to be affected as well.
6. Contractures:
- In advanced cases, the inflammation and thickening of the fascia can lead to contractures, which are permanent joint deformities characterized by limited mobility.
7. Reddened or Warm Skin:
- Affected areas may appear reddened and feel warm to the touch due to inflammation.
8. Nail Changes:
- Some individuals with EF may experience nail changes, such as nail bed thickening and nail plate deformation.
9. Hair Loss:
- Hair loss over affected areas of the skin or changes in hair texture may occur in some cases.
10. Systemic Symptoms: – Some individuals may experience systemic symptoms, such as fatigue, malaise, and generalized discomfort.
In summary, the symptoms and manifestations of Eosinophilic Fasciitis primarily involve pain, swelling, skin changes, and limited joint mobility, often accompanied by elevated eosinophil levels in the blood. Recognizing these symptoms is crucial for timely diagnosis and management of this rare connective tissue disorder.
Diagnosis
Diagnosing eosinophilic fasciitis typically involves a combination of clinical evaluation and diagnostic tests, including:
- Blood Tests: A blood test to measure eosinophil levels can help in diagnosing EF, as elevated eosinophils are a characteristic feature.
- Imaging Studies: X-rays, magnetic resonance imaging (MRI), and ultrasound may be used to assess the extent of fascial thickening and identify any joint involvement.
- Skin Biopsy: A biopsy of affected skin and fascia can confirm the presence of eosinophilic infiltrates.
Treatment Options
The treatment of eosinophilic fasciitis aims to manage symptoms, control inflammation, and improve joint mobility. Common treatment options include:
- Corticosteroids: High-dose corticosteroids are often the first-line treatment to reduce inflammation and relieve symptoms.
- Immunosuppressive Medications: In some cases, immunosuppressive drugs, such as methotrexate or mycophenolate mofetil, may be used to control the autoimmune response.
- Physical Therapy: Physical therapy and exercises can help maintain joint flexibility and prevent contractures.
- Pain Management: Pain management techniques, such as non-steroidal anti-inflammatory drugs (NSAIDs) or analgesics, may be used to alleviate discomfort.
here are key points about the treatment options for Eosinophilic Fasciitis (EF):
1. Corticosteroids:
- High-dose corticosteroids, such as prednisone, are often the initial treatment for EF.
- Corticosteroids help reduce inflammation and alleviate symptoms, including pain and skin changes.
2. Immunosuppressive Medications:
- In cases where corticosteroids alone are insufficient or for long-term management, immunosuppressive drugs may be prescribed.
- Medications like methotrexate or mycophenolate mofetil can help control the autoimmune response in EF.
3. Physical Therapy:
- Physical therapy is a vital component of EF treatment, aimed at maintaining joint flexibility and preventing contractures.
- It helps individuals regain mobility and improve their overall quality of life.
4. Pain Management:
- Pain management techniques, such as non-steroidal anti-inflammatory drugs (NSAIDs) or analgesics, may be used to alleviate discomfort and pain associated with EF.
5. Phototherapy:
- In some cases, phototherapy using ultraviolet (UV) light may be considered to reduce skin symptoms and inflammation.
6. Disease-Modifying Antirheumatic Drugs (DMARDs):
- DMARDs like hydroxychloroquine have been used in the treatment of EF to reduce skin thickening and inflammation.
7. Supportive Care:
- Supportive care measures, such as cool compresses, elevating affected limbs, and maintaining good skin hygiene, can help alleviate skin-related symptoms.
8. Splinting:
- In cases of joint contractures, splinting may be necessary to prevent further loss of mobility and improve joint function.
9. Psychological Support:
- EF can have a significant impact on an individual’s mental well-being. Psychological support and counseling can help individuals cope with the challenges of living with this rare condition.
10. Long-Term Management: – EF often requires long-term management to control symptoms and prevent relapses. Regular follow-up with healthcare providers is essential.
11. Research and Clinical Trials: – As EF is a rare and poorly understood condition, individuals and healthcare providers may explore participation in clinical trials and research studies to explore emerging treatment options.
In summary, the treatment of Eosinophilic Fasciitis involves a combination of medications, physical therapy, pain management, and supportive care to alleviate symptoms, control inflammation, and improve joint mobility. The choice of treatment may vary based on the severity of the condition and individual response, emphasizing the importance of individualized care and ongoing monitoring.
Prognosis
The prognosis for individuals with eosinophilic fasciitis can vary. Early diagnosis and prompt treatment are associated with better outcomes, and many individuals experience a reduction in symptoms and improved joint function. However, in some cases, EF may become chronic, leading to persistent symptoms and functional limitations.
Conclusion
Eosinophilic Fasciitis is a rare and enigmatic connective tissue disorder that can significantly impact an individual’s quality of life. While the exact cause remains unclear, advances in medical care and treatments, including corticosteroids and immunosuppressive medications, offer hope for symptom management and improved outcomes. Early diagnosis, proper medical care, and ongoing research are vital in enhancing our understanding of eosinophilic fasciitis and improving the care provided to those living with this rare condition.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023