Esophageal Cancer: A Human Perspective
Introduction:
In the intricate tapestry of human health, esophageal cancer emerges as a formidable challenge, demanding our attention and understanding. This article seeks to unravel the complexities surrounding esophageal cancer, exploring its nuances, risk factors, symptoms, and the avenues of treatment available to those grappling with this diagnosis.
Understanding Esophageal Cancer:
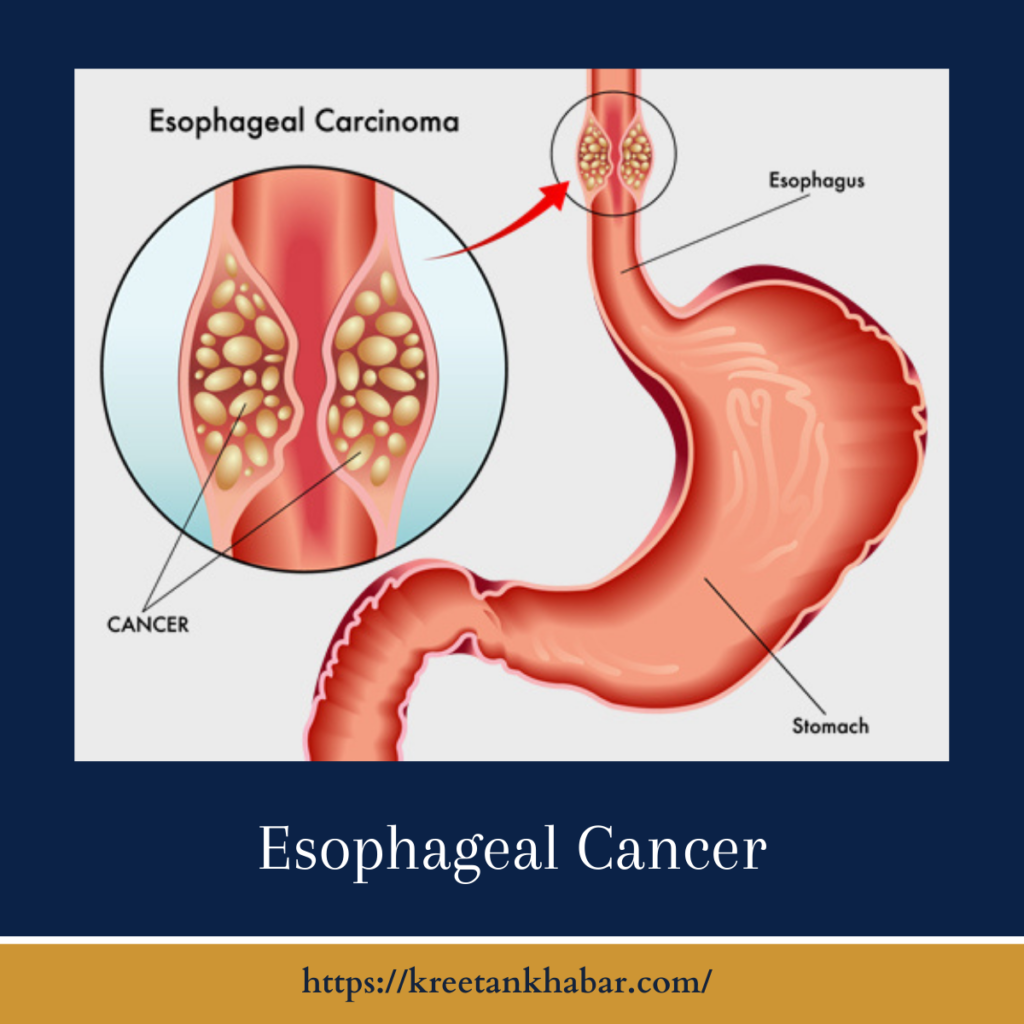
Esophageal cancer (also known as Oesophageal cancer) manifests in the tissues lining the esophagus, the muscular tube connecting the throat to the stomach. While it may not be as prevalent as some other cancers, its impact can be profound, prompting a closer examination of its causes, symptoms, and potential courses of action.
Risk Factors:
Several factors contribute to the development of esophageal cancer, emphasizing the importance of awareness and proactive health management. Common risk factors include chronic acid reflux or gastroesophageal reflux disease (GERD), tobacco use, excessive alcohol consumption, obesity, and a diet low in fruits and vegetables. Understanding these risk factors can empower individuals to make informed lifestyle choices.
Symptoms and Early Detection:
Esophageal cancer often progresses silently in its early stages, making early detection challenging. However, certain symptoms should prompt individuals to seek medical evaluation. These include difficulty swallowing, unexplained weight loss, persistent indigestion or heartburn, and discomfort or pain behind the breastbone. Acknowledging and addressing these symptoms in a timely manner is crucial for a prompt diagnosis.
Diagnosis:
The diagnostic journey for esophageal cancer typically begins with a thorough medical history and physical examination. To confirm the presence of cancer and understand its extent, various diagnostic tools may be employed. Endoscopy, where a flexible tube with a camera is inserted into the esophagus, allows for visual inspection and the collection of tissue samples for biopsy.
Imaging studies such as CT scans, PET scans, and barium swallow tests play a pivotal role in assessing the size and spread of the cancer. Through a collaborative effort involving gastroenterologists, oncologists, and radiologists, healthcare providers strive to form a comprehensive understanding of the individual’s condition.
Types of Esophageal Cancer:
Esophageal cancer is broadly classified into two main types: adenocarcinoma and squamous cell carcinoma. Adenocarcinoma typically arises in the cells lining the lower part of the esophagus, often linked to chronic acid reflux. Squamous cell carcinoma, on the other hand, usually develops in the cells lining the upper and middle parts of the esophagus, often associated with tobacco and alcohol use.
Treatment Options:
The approach to treating esophageal cancer is multifaceted, tailored to the individual’s specific circumstances. Treatment modalities may include surgery, chemotherapy, radiation therapy, or a combination of these. Surgical interventions may involve removing part or all of the esophagus, and in some cases, nearby lymph nodes.
Chemotherapy and radiation therapy may be employed to shrink tumors before surgery, eliminate remaining cancer cells post-surgery, or manage symptoms in cases where a cure is not feasible. Advances in medical research also bring forth targeted therapies, focusing on specific molecules involved in cancer growth.
Living with Esophageal Cancer:
A diagnosis of esophageal cancer not only impacts the physical well-being of individuals but also poses emotional and psychological challenges. Support from healthcare professionals, friends, and family becomes invaluable in navigating this complex journey. Dietary and lifestyle adjustments, as well as participation in support groups, can contribute to a holistic approach to living with and managing esophageal cancer.
Conclusion:
Esophageal cancer, with its intricate web of risk factors, symptoms, and treatment options, underscores the importance of awareness and early intervention. By demystifying this condition, fostering open communication, and embracing a comprehensive approach to healthcare, individuals facing esophageal cancer can embark on their journey with resilience, hope, and a sense of empowerment.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023