Fatty Liver: Causes, Symptoms, and Treatment
Introduction
Fatty liver, also known as hepatic steatosis, is a common liver condition that affects millions of people worldwide. While it may not sound as serious as other liver diseases, such as cirrhosis or hepatitis, it’s a condition that deserves attention due to its potential health implications. In this article, we will delve into the world of fatty liver, exploring its causes, symptoms, and treatment options.
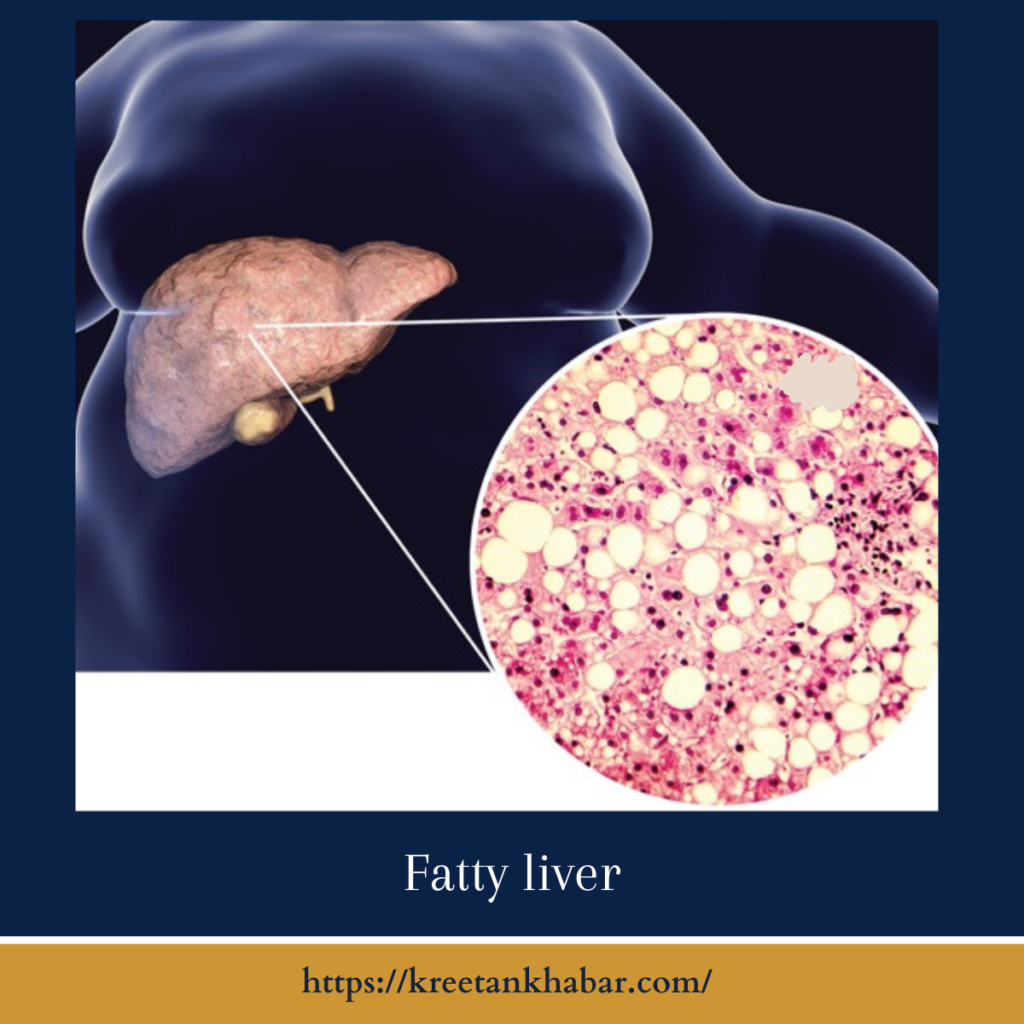
What is Fatty Liver?
Fatty liver is a condition where excess fat accumulates in the liver cells. The liver is responsible for various essential functions, such as processing nutrients, detoxifying the body, and producing vital proteins. When too much fat accumulates in the liver, it can interfere with these processes, potentially leading to liver damage and other health complications.
Causes of Fatty Liver
- Non-Alcoholic Fatty Liver Disease (NAFLD): This is the most common cause of fatty liver and is not related to excessive alcohol consumption. NAFLD is often associated with obesity, insulin resistance, and metabolic syndrome.
- Alcoholic Fatty Liver Disease: As the name suggests, this type of hepatic steatosis is caused by excessive alcohol consumption. It can range from mild to severe, and its severity is linked to the amount and duration of alcohol intake.
- Medications and Toxins: Certain medications and exposure to toxins can lead to hepatic steatosis. Some examples include corticosteroids, tamoxifen, and tetracycline antibiotics.
- Rapid Weight Loss: Losing a significant amount of weight in a short period can lead to the release of fat into the liver, causing hepatic steatosis.
- Genetics: Some individuals may be genetically predisposed to fatty liver, making them more susceptible to the condition even without other risk factors.
Here are some key points about the causes of fatty liver:
- Non-Alcoholic Fatty Liver Disease (NAFLD): This is the most common cause of fatty liver and is not linked to excessive alcohol consumption. It is often associated with obesity, insulin resistance, and metabolic syndrome.
- Alcoholic Fatty Liver Disease: Excessive alcohol consumption can lead to the accumulation of fat in the liver. The severity of this condition is directly related to the amount and duration of alcohol intake.
- Medications and Toxins: Certain medications and exposure to toxins can trigger fatty liver. Medications like corticosteroids, tamoxifen, and tetracycline antibiotics are known culprits.
- Rapid Weight Loss: Losing a significant amount of weight quickly can release fat into the liver, causing fatty liver. This is often seen in crash diets or bariatric surgery patients.
- Genetics: Some individuals may be genetically predisposed to fatty liver, making them more susceptible to the condition, even without other risk factors.
- Insulin Resistance: Insulin resistance, often associated with type 2 diabetes, can increase the likelihood of developing hepatic steatosis as it affects how the liver processes fats.
- High Sugar and High-Fat Diet: Consuming a diet high in sugars and unhealthy fats can contribute to the development of hepatic steatosis, particularly in the context of insulin resistance.
- Sedentary Lifestyle: Lack of physical activity and a sedentary lifestyle can promote fat accumulation in the liver, especially when combined with poor dietary choices.
- Pregnancy: Some women may develop a condition called gestational diabetes during pregnancy, which can increase the risk of hepatic steatosis.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that can be associated with insulin resistance, making women with PCOS more prone to hepatic steatosis.
- Infections: In rare cases, viral hepatitis, like hepatitis C, can lead to hepatic steatosis as the liver becomes inflamed and unable to process fats normally.
Understanding the various causes of hepatic steatosis is crucial in addressing the condition effectively. Identifying the underlying cause is the first step in developing a suitable treatment plan and making necessary lifestyle changes to manage or prevent fatty liver disease.
Symptoms of Fatty Liver
Fatty liver is often considered a silent condition, as it may not produce noticeable symptoms in its early stages. When symptoms do appear, they can be non-specific and may include:
- Fatigue
- Pain in the upper right abdomen
- Abdominal swelling
- Jaundice (yellowing of the skin and eyes)
- Unexplained weight loss
It’s important to note that these symptoms can be associated with other health issues as well, so a proper diagnosis is essential.
Diagnosis and Treatment
Diagnosing hepatic steatosis usually begins with a physical examination and a discussion of medical history. Physicians may also employ various diagnostic tests, including blood tests, imaging studies (ultrasound, CT scan, MRI), and liver biopsy to confirm the diagnosis and determine the severity of the condition.
Treatment for hepatic steatosis depends on its underlying cause and severity. Here are some general approaches:
- Lifestyle Changes: For NAFLD, lifestyle modifications are often the first line of treatment. This may include weight loss, dietary changes, and increased physical activity.
- Alcohol Abstinence: If alcoholic hepatic steatosis disease is the culprit, complete abstinence from alcohol is crucial. Support and counseling may be needed to achieve and maintain sobriety.
- Medication: In some cases, medications may be prescribed to manage underlying conditions such as diabetes, high cholesterol, or obesity, which can contribute tohepatic steatosis.
- Regular Monitoring: It’s essential for individuals with hepatic steatosis to have regular check-ups with their healthcare providers to monitor the progression of the disease and adjust treatment as needed.
Here are some key points about the diagnosis and treatment of hepatic steatosis:
Diagnosis of Fatty Liver:
- Medical History: A diagnosis often begins with a thorough review of the patient’s medical history, including any risk factors and symptoms.
- Physical Examination: During a physical exam, a healthcare provider may check for signs of an enlarged liver or abdominal tenderness.
- Blood Tests: Blood tests can help determine liver enzyme levels, presence of liver inflammation, and rule out other liver diseases.
- Imaging Studies: Ultrasound, CT scans, or MRI can provide detailed images of the liver, revealing the presence and extent of fatty deposits.
- Liver Biopsy: In some cases, a liver biopsy may be recommended to assess the severity of the condition. A small sample of liver tissue is collected for examination.
Treatment of Fatty Liver:
- Lifestyle Changes: For non-alcoholic hepatic steatosis disease (NAFLD), the cornerstone of treatment involves lifestyle modifications. This includes:
- Weight Loss: Achieving and maintaining a healthy weight can reduce fat accumulation in the liver. Gradual weight loss is typically recommended.
- Dietary Changes: Adopting a balanced diet that is low in saturated fats, sugars, and processed foods can improve liver health. Increased consumption of fruits, vegetables, and whole grains is encouraged.
- Physical Activity: Regular exercise is crucial in managing hepatic steatosis. Aerobic exercise and strength training can help improve insulin sensitivity and reduce fat in the liver.
- Alcohol Abstinence: For alcoholic hepatic steatosis disease, complete abstinence from alcohol is essential. Support and counseling may be necessary to help individuals achieve and maintain sobriety.
- Medications: In some cases, medications may be prescribed to manage underlying conditions that contribute to hepatic steatosis, such as diabetes, high cholesterol, or obesity.
- Regular Monitoring: Individuals with fatty liver should have regular check-ups with their healthcare providers to monitor the progression of the disease and make necessary adjustments to treatment plans.
- Manage Underlying Conditions: If fatty liver is related to other health issues like insulin resistance or high blood pressure, these conditions need to be effectively managed.
- Liver Transplant (in severe cases): In extremely rare and severe cases where hepatic steatosis progresses to non-alcoholic steatohepatitis (NASH) and causes liver failure, a liver transplant may be considered.
- Preventive Measures: Preventing the underlying causes of fatty liver, such as maintaining a healthy weight, limiting alcohol consumption, and managing diabetes, can help prevent the condition from developing or worsening.
The diagnosis and treatment of hepatic steatosis depend on the specific type (non-alcoholic or alcoholic) and the individual’s overall health. An accurate diagnosis and a tailored treatment plan are essential to managing this condition effectively and preventing it from progressing to more severe liver diseases.
Conclusion
Fatty liver is a prevalent condition with various underlying causes, and it can lead to serious health complications if left untreated. However, with the right approach, including lifestyle changes, appropriate medical care, and early diagnosis, it can often be managed effectively. If you suspect you may have fatty liver or are at risk, it’s important to consult with a healthcare professional for guidance and support in maintaining your liver health. Remember, a healthy liver is vital for overall well-being.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023