Frozen Shoulder and Finding Relief
Introduction:
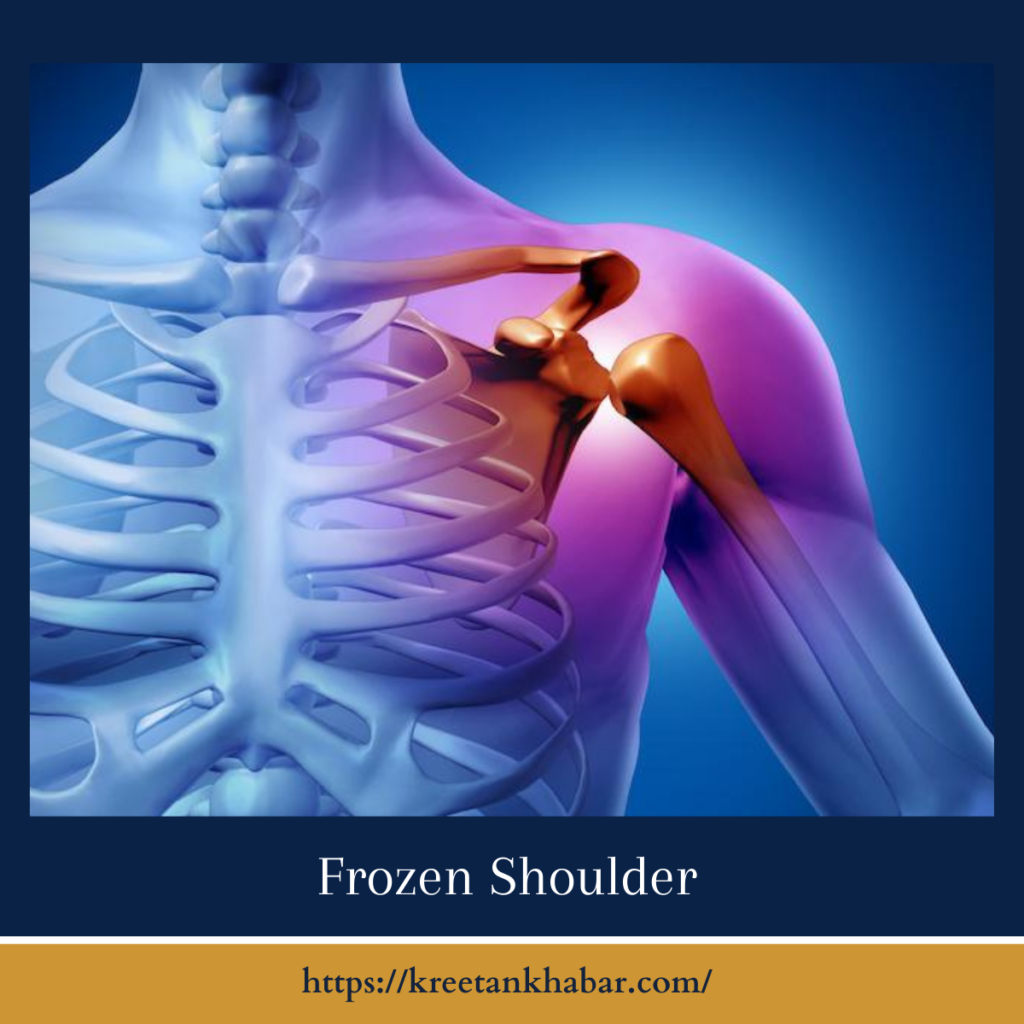
Imagine waking up one morning to find that moving your shoulder has become an excruciating task, with each movement met by intense pain and stiffness. This scenario is all too familiar for individuals suffering from frozen shoulder(also known as Adhesive Capsulitis), a debilitating condition that can severely limit mobility and impact daily life. In this article, we’ll explore the complexities of frozen shoulder, including its causes, symptoms, diagnosis, and treatment options, to provide insight into this common yet often misunderstood shoulder disorder.
Understanding Frozen Shoulder:
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by stiffness, pain, and limited range of motion in the shoulder joint. While the exact cause of frozen shoulder remains unclear, it is believed to involve inflammation, thickening, and tightening of the shoulder joint capsule, the connective tissue surrounding the shoulder joint. This results in the formation of adhesions or scar tissue within the joint capsule, leading to decreased flexibility and mobility of the shoulder.
Symptoms of Frozen Shoulder:
The hallmark symptoms of Adhesive Capsulitis typically develop gradually and progress through three distinct stages:
- Freezing Stage: During this initial stage, individuals experience a gradual onset of shoulder pain and stiffness, which worsens over time. Range of motion in the shoulder joint becomes increasingly limited, making simple tasks such as reaching overhead or behind the back challenging and painful.
- Frozen Stage: In the frozen stage, shoulder stiffness and pain reach their peak, with significant restrictions in shoulder mobility. Activities that require lifting, reaching, or rotating the arm become nearly impossible, leading to functional limitations and decreased quality of life.
- Thawing Stage: The thawing stage marks the gradual improvement of symptoms, with a gradual return of shoulder mobility and a reduction in pain. While the thawing stage can last several months to years, most individuals experience significant improvement in shoulder function over time.
Causes and Risk Factors:
While the precise cause of Adhesive Capsulitis remains unclear, several factors may contribute to its development, including:
- Age: Frozen shoulder most commonly affects individuals between the ages of 40 and 60, with the risk increasing with age.
- Gender: Women are more likely than men to develop Adhesive Capsulitis, particularly postmenopausal women.
- Medical Conditions: Certain medical conditions such as diabetes, thyroid disorders, heart disease, and Parkinson’s disease have been associated with an increased risk of developing frozen shoulder.
- Shoulder Trauma or Surgery: Previous shoulder injuries, trauma, or surgery can predispose individuals to develop Adhesive Capsulitis, as inflammation and scarring within the shoulder joint may contribute to the development of adhesive capsulitis.
- Immobility or Inactivity: Prolonged periods of immobility or inactivity, such as during recovery from surgery or due to illness or injury, can increase the risk of developing frozen shoulder.
Diagnosis and Treatment:
Diagnosing frozen shoulder typically involves a thorough medical history, physical examination, and imaging studies such as X-rays or magnetic resonance imaging (MRI) to rule out other shoulder conditions and confirm the diagnosis. Treatment for frozen shoulder aims to relieve pain, improve shoulder mobility, and restore function and may include:
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, or oral pain medications may be prescribed to alleviate pain and inflammation.
- Physical Therapy: Physical therapy exercises and stretches can help improve shoulder mobility, strengthen surrounding muscles, and reduce stiffness.
- Joint Mobilization: Manual therapy techniques such as joint mobilization or manipulation performed by a qualified healthcare professional can help break up adhesions and improve shoulder range of motion.
- Hydrodilatation: In some cases, a procedure known as hydrodilatation may be performed, where a sterile saline solution is injected into the shoulder joint to stretch the capsule and improve mobility.
- Surgical Intervention: In severe cases of frozen shoulder that do not respond to conservative treatment, surgical intervention such as arthroscopic capsular release may be considered to release adhesions and improve shoulder mobility.
Conclusion:
Frozen shoulder is a painful and debilitating condition that can significantly impact an individual’s quality of life. While the exact cause of frozen shoulder remains unclear, early diagnosis and prompt treatment can help alleviate symptoms, improve shoulder mobility, and restore function. By understanding the causes, symptoms, and treatment options for frozen shoulder, individuals and healthcare professionals alike can work together to effectively manage this common shoulder disorder and help individuals regain control of their shoulder health and overall well-being.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023