Gastro-Oesophageal Reflux Disease (GERD): Understanding the Causes, Symptoms, and Effective Management
Introduction
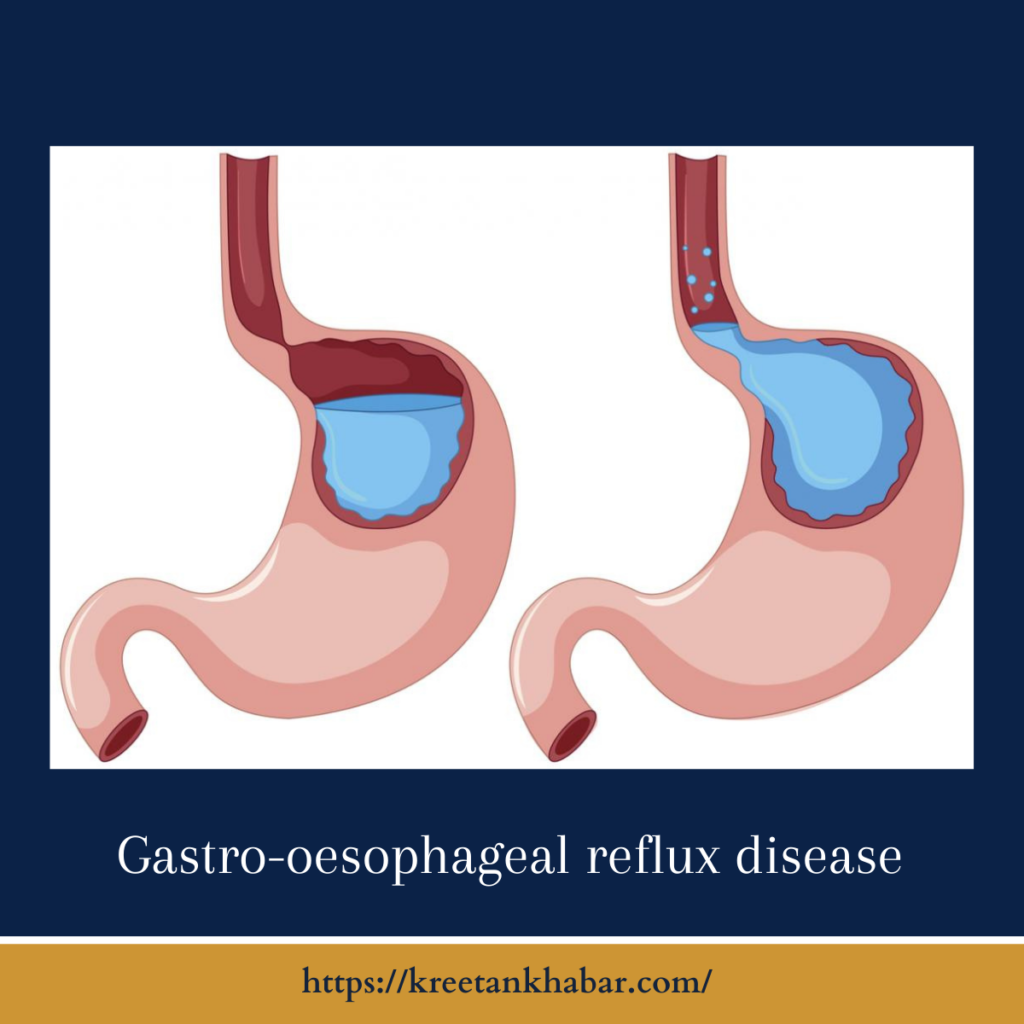
Gastro-oesophageal reflux disease, commonly referred to as GERD, is a chronic digestive disorder that affects millions of people worldwide. It occurs when stomach acid frequently flows back into the oesophagus, causing irritation and a range of uncomfortable symptoms. In this article, we’ll delve into the world of GERD, exploring its causes, symptoms, and strategies for effective management.
Understanding GERD
GERD is a chronic condition characterized by the frequent and persistent backflow of stomach acid into the oesophagus. The lower oesophageal sphincter (LES), a muscular ring that acts as a barrier between the oesophagus and the stomach, becomes weakened or relaxed in individuals with Gastro-oesophageal reflux disease, allowing stomach acid to escape into the oesophagus.
Common Causes of GERD
- Hiatal Hernia: A hiatal hernia occurs when a portion of the stomach bulges through the diaphragm, increasing the risk of Gastro-oesophageal reflux disease.
- Obesity: Excess body weight can put pressure on the abdomen, forcing stomach acid into the oesophagus.
- Pregnancy: Hormonal changes and increased pressure on the abdomen during pregnancy can lead to Gastro-oesophageal reflux disease.
- Smoking: Smoking weakens the LES and can contribute to Gastro-oesophageal reflux disease development.
- Certain Foods: Spicy, acidic, or fatty foods, as well as caffeine and alcohol, can trigger or exacerbate Gastro-oesophageal reflux disease symptoms.
- Medications: Some medications, such as calcium channel blockers, antihistamines, and certain asthma medications, can relax the LES, increasing the risk of Gastro-oesophageal reflux disease.
- Eating Large Meals: Consuming large meals or lying down immediately after eating can promote acid reflux.
Common Symptoms of GERD
- Heartburn: A burning sensation or discomfort in the chest, often after eating or when lying down.
- Regurgitation: The sensation of stomach acid or partially digested food flowing into the throat or mouth.
- Dysphagia: Difficulty swallowing or a sensation of food sticking in the throat.
- Chronic Cough: A persistent dry cough, often worsened at night or after meals.
- Sore Throat: Repeated exposure to stomach acid can lead to throat irritation and a sore throat.
- Hoarseness: Chronic irritation can affect the vocal cords, resulting in hoarseness.
- Asthma: GERD can exacerbate asthma symptoms or trigger asthma attacks in some individuals.
Effective Management of GERD
- Lifestyle Modifications: Adopting certain lifestyle changes can help manage Gastro-oesophageal reflux disease, including weight loss, avoiding trigger foods, and eating smaller, more frequent meals.
- Elevate the Head of the Bed: Raising the head of your bed by 6 to 8 inches can prevent acid from flowing into the oesophagus during sleep.
- Medications: Over-the-counter antacids and acid-reducing medications can provide relief. In severe cases, prescription medications may be necessary.
- Avoid Eating Late at Night: Allow at least 2-3 hours between your last meal and bedtime to prevent nighttime reflux.
- Quit Smoking: If you smoke, quitting can improve LES function and reduce Gastro-oesophageal reflux disease symptoms.
- Stress Reduction: Techniques such as yoga, meditation, and deep breathing exercises can help manage stress, which can exacerbate Gastro-oesophageal reflux disease.
- Surgery: In severe cases where lifestyle changes and medications aren’t effective, surgical procedures like fundoplication may be considered to strengthen the LES.
Here are points outlining effective management strategies for Gastro-oesophageal reflux disease (GERD):
- Lifestyle Modifications: Implement lifestyle changes to reduce Gastro-oesophageal reflux disease symptoms. These include:
- Dietary Adjustments: Avoid trigger foods such as spicy, acidic, or fatty items, caffeine, and alcohol.
- Smaller Meals: Opt for smaller, more frequent meals to reduce stomach pressure and acid reflux.
- Weight Management: Achieve and maintain a healthy weight to alleviate pressure on the abdomen.
- Posture During Meals: Sit upright while eating and avoid lying down immediately after meals.
- Elevate the Head of the Bed: Raise the head of your bed by 6 to 8 inches using bed risers or blocks to prevent nighttime reflux.
- Medications: Over-the-counter antacids, H2 blockers, or proton pump inhibitors (PPIs) can be used to reduce acid production and provide relief. Prescription-strength medications may be needed for severe cases.
- Timing of Meals: Allow 2-3 hours between your last meal and bedtime to minimize nighttime reflux.
- Quit Smoking: Smoking weakens the lower oesophageal sphincter (LES), so quitting can improve LES function and reduce Gastro-oesophageal reflux disease symptoms.
- Stress Reduction: Practice stress management techniques such as meditation, deep breathing, and yoga, as stress can exacerbate Gastro-oesophageal reflux disease symptoms.
- Avoid Tight Clothing: Wear loose-fitting clothing, especially around the waist, to prevent abdominal pressure.
- Chew Gum: Chewing sugar-free gum after meals can stimulate saliva production, which helps neutralize acid.
- Baking Soda: In moderation, a teaspoon of baking soda dissolved in water can act as an antacid.
- Sleep Position: Sleep on your left side to reduce reflux symptoms, as it may prevent the junction between the stomach and oesophagus from opening as easily.
- Hydration: Stay well-hydrated with water to help dilute stomach acid.
- Avoid Trigger Beverages: Limit or avoid carbonated beverages, citrus juices, and alcohol.
- Maintain a Food Diary: Keep a diary to identify specific foods or drinks that trigger your Gastro-oesophageal reflux disease symptoms.
- Regular Exercise: Engage in regular, moderate exercise to maintain a healthy weight and reduce the risk of Gastro-oesophageal reflux disease.
- Dental Hygiene: Practice good dental hygiene to prevent tooth erosion caused by stomach acid.
- Regular Follow-ups: Attend regular check-ups with your healthcare provider to monitor Gastro-oesophageal reflux disease and adjust your treatment plan if necessary.
- Prescription Medications: If over-the-counter medications are ineffective, consult your healthcare provider for prescription-strength options or alternative medications.
- Surgery: In severe cases, surgical procedures like fundoplication may be considered to strengthen the LES and prevent reflux.
- Monitor Symptoms: Pay attention to symptom patterns, triggers, and severity, and share this information with your healthcare provider.
- Raise the Bed Safely: Elevate the head of the bed using proper supports to ensure safety during sleep.
- Avoid Late-Night Snacking: Refrain from eating snacks or heavy meals close to bedtime.
- Consult a Registered Dietitian: A registered dietitian can provide personalized dietary guidance tailored to your Gastro-oesophageal reflux disease symptoms and triggers.
- Follow Medication Instructions: If prescribed medications, adhere to the recommended dosage and schedule.
- Watch for Complications: Be vigilant for complications like Barrett’s oesophagus or strictures, and seek immediate medical attention if you experience severe symptoms.
- Discuss Surgical Options: If lifestyle changes and medications are ineffective, consult a specialist to discuss surgical interventions.
- Consider Non-Medical Therapies: Explore complementary therapies like acupuncture or dietary supplements under the guidance of a healthcare provider.
Effective management of Gastro-oesophageal reflux disease often involves a combination of these strategies, tailored to your individual needs and the severity of your condition. Always consult with a healthcare provider for a proper diagnosis and personalized treatment plan.
Conclusion
GERD is a chronic digestive disorder that can significantly impact one’s quality of life. Understanding its causes, recognizing its symptoms, and implementing effective management strategies are essential steps in minimizing discomfort and preventing complications. If you suspect you have Gastro-oesophageal reflux disease or experience persistent symptoms, consult a healthcare provider for a proper diagnosis and personalized treatment plan.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023