Understanding Genital Warts: Causes, Symptoms, Treatment, and Prevention
Introduction
Genital warts, also known as condylomata acuminata, are a common sexually transmitted infection (STI) caused by specific strains of the human papillomavirus (HPV). These warts can affect the genital and anal areas, and while they are typically harmless, they can cause discomfort and concern. This article aims to provide insights into genital warts, including their causes, symptoms, treatment, and preventive measures.
Causes of Genital Warts
- HPV Infection: condylomata acuminata Genital warts are primarily caused by HPV infection. HPV is a group of viruses, and certain high-risk strains can lead to the development of genital warts.
- Sexual Contact: Genital warts are primarily transmitted through sexual contact, including vaginal, anal, and oral sex. They can be spread from one person to another even when there are no visible warts.
- Skin-to-Skin Contact: Genital warts can also be spread through skin-to-skin contact with an infected person, even if sexual intercourse does not occur.
- Multiple Partners: Having multiple sexual partners increases the risk of HPV infection and, subsequently, condylomata acuminata.
Symptoms of Genital Warts
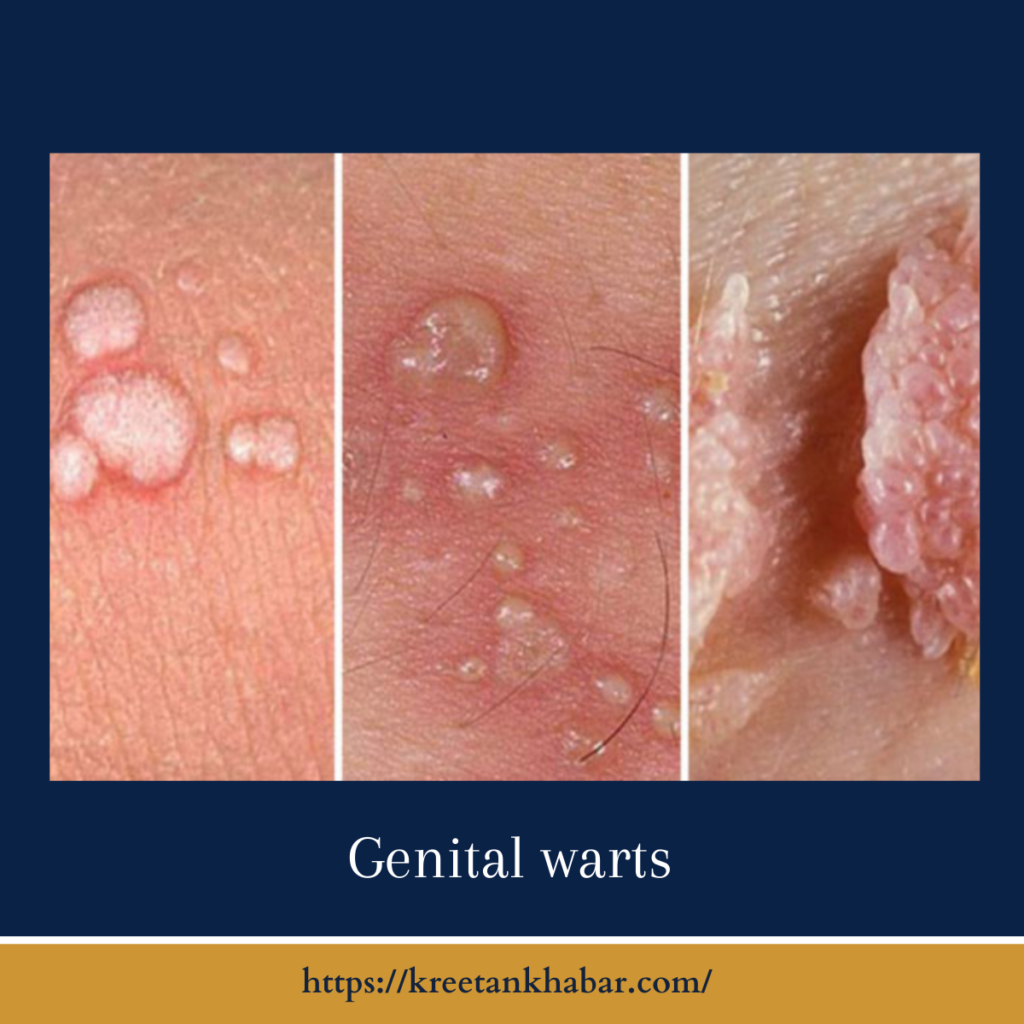
- Warts: The most recognizable symptom of genital warts is the presence of small, flesh-colored or gray growths in the genital and anal areas. These warts can be flat, raised, or cauliflower-shaped.
- Itching and Discomfort: condylomata acuminata can cause itching, discomfort, or a burning sensation, especially if they appear in areas with friction, such as during sexual activity.
- Bleeding: In some cases, condylomata acuminata may bleed, particularly when irritated or during sexual intercourse.
- Clustering: Warts may appear in clusters or individually and can vary in size from barely noticeable to larger growths.
- Location: Genital warts can occur on the vulva, vagina, cervix, penis, scrotum, anus, or in the groin area.
ere are points outlining the common symptoms of genital warts:
Symptoms of Genital Warts:
- Visible Warts: The hallmark symptom of genital warts is the presence of small, flesh-colored or gray growths in the genital and anal areas. These warts can appear in various shapes, including flat, raised, or resembling cauliflower-like clusters.
- Genital and Anal Location: Genital warts typically occur on or around the genitalia, including the vulva, vagina, cervix, penis, scrotum, and anus. They may also be found in the groin area.
- Size Variation: Genital warts can vary in size, from tiny growths that are barely noticeable to larger, more prominent warts.
- Itching: Many individuals with genital warts experience itching or discomfort in the affected areas. This itching may become more pronounced if the warts are irritated or during sexual activity.
- Bleeding: Genital warts can sometimes bleed, particularly if they are scratched, rubbed, or irritated.
- Pain or Burning: In some cases, condylomata acuminata may cause a burning sensation or mild pain, especially during sexual intercourse or when pressure is applied.
- Clustering: Warts may appear individually or in clusters, often resembling a cluster of miniature cauliflowers.
- Changes Over Time: condylomata acuminata can evolve and change in appearance over time. They may grow, shrink, or disappear on their own.
- Asymptomatic: Some individuals infected with HPV may not exhibit any visible symptoms, making regular screening and safe sexual practices crucial for early detection and prevention.
It’s important to remember that not all condylomata acuminata are visible to the naked eye, and some may be internal or not readily noticeable. If you suspect you have genital warts or have been exposed to HPV, it is advisable to consult with a healthcare provider for proper diagnosis, treatment, and guidance on managing the condition.
Treatment of Genital Warts
- Topical Medications: Healthcare providers may prescribe topical creams or ointments containing imiquimod or podofilox to apply directly to the warts. These medications help stimulate the immune system to fight the virus.
- Cryotherapy: Cryotherapy involves freezing the warts with liquid nitrogen. This treatment causes the warts to slough off as the skin heals.
- Electrocautery: Electrocautery uses an electrical current to burn off the warts. It is typically done in a healthcare provider’s office.
- Surgical Removal: Large or stubborn warts may require surgical removal, which can be done through excision, laser therapy, or electrocautery.
- Prescription Medications: Some cases may require prescription medications, such as trichloroacetic acid (TCA), to destroy the warts.
- Regular Monitoring: condylomata acuminata may reappear after treatment, and regular follow-up visits to a healthcare provider are crucial.
ere are points outlining the treatment options for genital warts:
Treatment of Genital Warts:
- Medical Evaluation: If you suspect you have condylomata acuminata or have been diagnosed with them, consult a healthcare provider for a comprehensive evaluation and personalized treatment plan.
- Topical Medications: Healthcare providers often prescribe topical medications containing imiquimod or podofilox. These creams or ointments are applied directly to the warts and work to stimulate the body’s immune response to fight the virus. Patients are typically instructed on how to apply these medications at home.
- Cryotherapy: Cryotherapy involves the use of liquid nitrogen to freeze and remove condylomata acuminata. A healthcare provider performs this procedure in a clinical setting. As the frozen warts thaw and heal, they slough off.
- Electrocautery: Electrocautery uses an electrical current to burn off the warts. This is a procedure performed by a healthcare provider, typically in an office or clinic.
- Surgical Removal: In cases of larger or stubborn warts, healthcare providers may recommend surgical removal. Surgical methods include excision (cutting out the warts), laser therapy (using laser to vaporize the warts), and electrocautery.
- Prescription Medications: In some instances, healthcare providers may prescribe prescription medications such as trichloroacetic acid (TCA) or podophyllin resin to be applied directly to the warts.
- Intralesional Interferon: For particularly challenging cases, healthcare providers may inject interferon directly into the warts to stimulate the immune system’s response to the virus.
- Regular Follow-Up: After treatment, regular follow-up appointments with a healthcare provider are essential to monitor the progress of treatment and assess for any recurrence of warts.
- Preventive Measures: During and after treatment, individuals should take measures to prevent further transmission of HPV, including practicing safe sex, using condoms, and getting vaccinated against HPV.
- Patient Education: Healthcare providers should educate patients about the importance of follow-up visits, safe sexual practices, and HPV vaccination.
It’s important to note that treatment effectiveness can vary depending on the size, location, and number of warts, as well as the individual’s overall health. Some genital warts may recur after treatment, and a comprehensive approach to managing HPV may involve ongoing monitoring and preventive measures. Always consult with a healthcare provider for the most suitable treatment plan tailored to your specific condition.
Prevention of Genital Warts
- Vaccination: The HPV vaccine is highly effective in preventing the most common high-risk HPV strains that cause genital warts and cervical cancer. It is recommended for both males and females.
- Safe Sex: Consistently and correctly using condoms can reduce the risk of HPV transmission, although they do not provide complete protection.
- Limit Sexual Partners: Reducing the number of sexual partners can lower the risk of HPV exposure.
- HPV Screening: Regular HPV screening and Pap smears for cervical cancer can help detect and manage HPV-related conditions, including genital warts.
- Avoidance: Abstaining from sexual activity is the only surefire way to avoid HPV infection.
Conclusion
Genital warts are a common and treatable STI caused by specific HPV strains. Early diagnosis and appropriate treatment can help manage the condition effectively. Preventive measures, including vaccination and safe sexual practices, are essential in reducing the risk of genital warts and other HPV-related conditions. It is important to consult with a healthcare provider for diagnosis, treatment, and guidance on preventing and managing genital warts.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023