Hendra Virus: A Deep Dive into Origins, Risks, and Prevention
Introduction:
In the intricate web of zoonotic viruses, Hendra virus (also known as Equine morbillivirus) emerges as a formidable player, raising concerns about the delicate balance between human and animal health. Named after the suburb in Brisbane, Australia, where it was first identified in 1994, Equine morbillivirus has sparked conversations and research efforts worldwide. This article aims to shed light on the Hendra virus, exploring its origins, the risks it poses, and crucial measures for prevention.
Understanding Hendra Virus:
- Origins and Reservoir Host:
Equine morbillivirus is a member of the Henipavirus genus, closely related to the Nipah virus. Its natural reservoir host is believed to be fruit bats (flying foxes), with spillover into horses and, on rare occasions, to humans. This complex transmission pathway underscores the importance of studying the dynamics between wildlife, domestic animals, and humans.
- Incidents and Outbreaks:
While Hendra virus incidents are relatively rare, they can have severe consequences. The virus gained global attention due to sporadic outbreaks in Australia, particularly in Queensland and New South Wales. Horses often serve as an intermediary host, contracting the virus from bats and transmitting it to humans.
- Human Infections:
Human infections with Equine morbillivirus are fortunately infrequent but carry a high mortality rate. The symptoms can range from respiratory distress to encephalitis, posing a significant public health concern.
Risks and Prevention:
- Occupational Risk:
Those working closely with horses, such as veterinarians, horse trainers, and handlers, face an increased risk of exposure. Adequate precautions, including personal protective equipment (PPE), are essential when dealing with potentially infected animals.
- Precautions for Horse Owners:
Horse owners can minimize the risk by implementing biosecurity measures. Isolating sick horses, avoiding close contact with bats, and maintaining proper hygiene are crucial steps in preventing Hendra virus transmission.
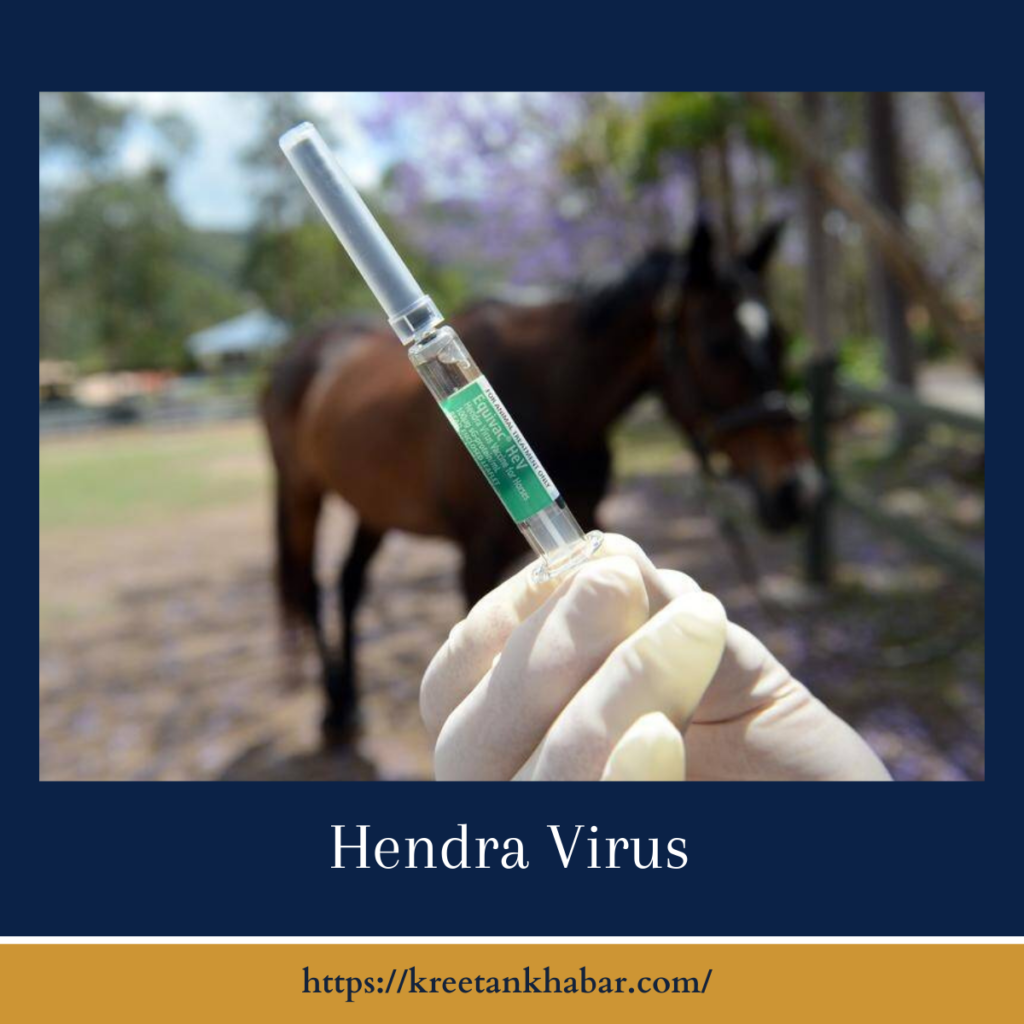
- Vaccination for Horses:
Vaccination is a pivotal tool in mitigating Hendra virus risks. A vaccine for horses has been developed, providing a protective barrier and reducing the likelihood of transmission to both humans and other horses.
- Public Health Awareness:
Raising awareness among the public about the risks associated with Hendra virus is crucial. Promoting responsible horse ownership and educating communities on preventive measures contribute to overall risk reduction.
- Wildlife Conservation:
Recognizing the role of fruit bats as reservoir hosts emphasizes the need for a holistic approach to wildlife conservation. Preserving natural habitats for bats while minimizing close interactions with humans and domestic animals is vital.
Conclusion:
Hendra virus stands as a testament to the intricate connections between animal and human health. While the risks associated with this virus are serious, ongoing research, public awareness, and preventive measures offer hope in mitigating its impact. The collaboration between the scientific community, healthcare professionals, and the public is instrumental in navigating the complexities of zoonotic diseases and fostering a harmonious coexistence between species.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023