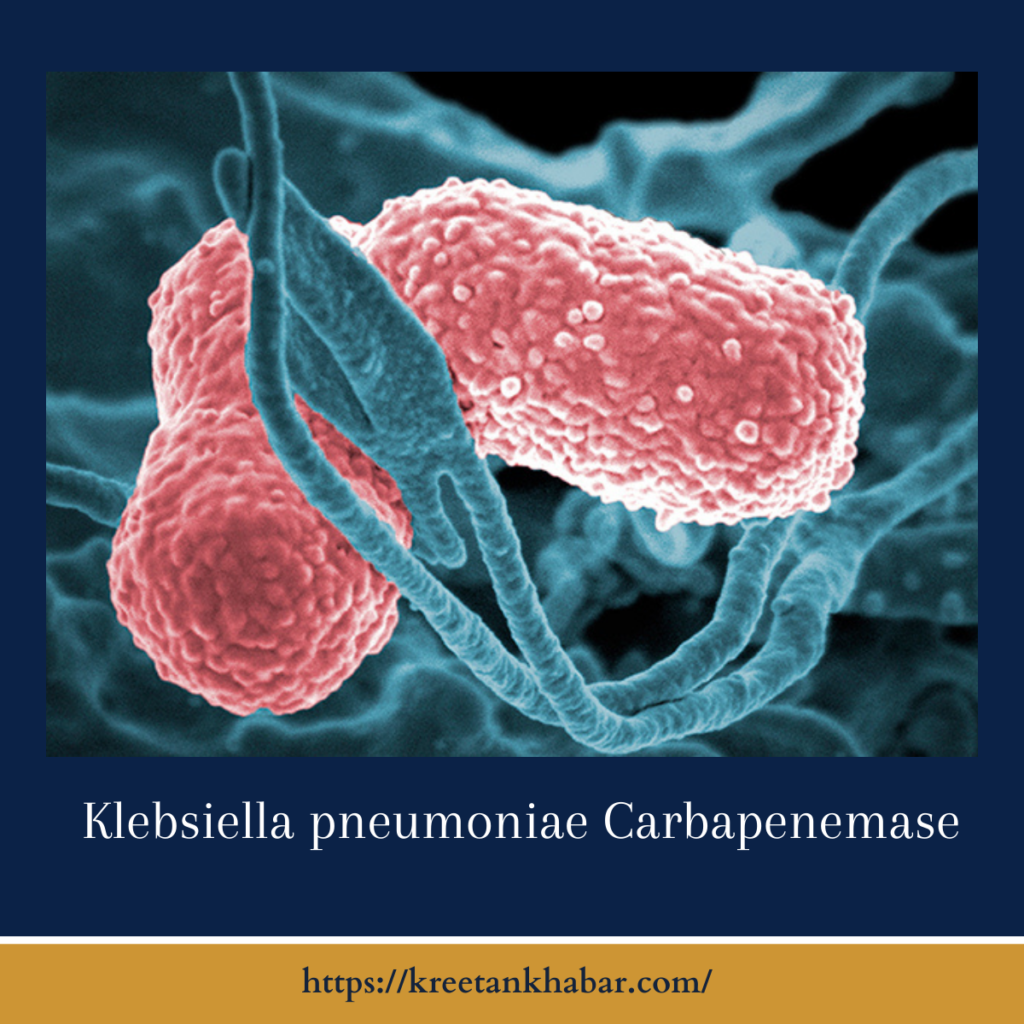
Klebsiella Pneumoniae Carbapenemase: A Rising Concern in Healthcare
Introduction:
In the intricate landscape of healthcare-associated infections, the emergence of Klebsiella pneumoniae carbapenemase (KPC) stands as a formidable challenge. This enzyme, produced by the bacterium Klebsiella pneumoniae, has garnered attention for its role in rendering antibiotics ineffective, particularly the potent class of carbapenems. In this article, we delve into the nuances of Klebsiella pneumoniae carbapenemase, exploring its origins, impact on healthcare, and the ongoing efforts to tackle this growing concern.
Understanding KPC:
- The Genesis of Resistance:
- Klebsiella pneumoniae, a common bacteria found in the human gastrointestinal tract, has developed the ability to produce the enzyme Klebsiella pneumoniae carbapenemase. This enzyme, classified as a carbapenemase, has the alarming capacity to break down carbapenem antibiotics, leaving medical professionals with limited options for treatment.
- Global Spread:
- What adds to the complexity of Klebsiella pneumoniae carbapenemase is its global spread. Cases have been reported across various continents, underscoring the importance of a coordinated international response to address this concerning phenomenon.
Impact on Healthcare:
- Treatment Dilemmas:
- The emergence of Klebsiella pneumoniae carbapenemase poses significant challenges in the realm of infectious disease management. Carbapenems, once considered a last line of defense against bacterial infections, are now compromised, leading to treatment dilemmas and increased reliance on alternative, often less effective, antibiotics.
- Hospital Outbreaks:
-
- KPC is often associated with hospital-acquired infections, leading to outbreaks within healthcare facilities. The ability of the bacterium to spread easily and the limited treatment options contribute to the persistence of Klebsiella pneumoniae carbapenemase in hospital settings.
Points of Impact on healthcare:
- Treatment Challenges:
- Klebsiella pneumoniae carbapenemase (KPC) presents significant challenges in healthcare by compromising the effectiveness of carbapenem antibiotics, traditionally considered powerful weapons against bacterial infections. This limitation complicates treatment strategies and increases the reliance on alternative, often less potent, antibiotics.
- Hospital-Acquired Infections:
- KPC is frequently associated with hospital-acquired infections, leading to outbreaks within healthcare facilities. The ability of Klebsiella pneumoniae to spread easily within a hospital setting poses a considerable risk, requiring stringent infection control measures.
- Limited Antibiotic Options:
- The emergence of Klebsiella pneumoniae carbapenemase restricts the antibiotic options available for treating infections caused by Klebsiella pneumoniae. The diminished effectiveness of carbapenems leaves healthcare providers with fewer choices, sometimes resorting to older or more toxic antibiotics.
- Increased Mortality Rates:
- Infections involving Klebsiella pneumoniae carbapenemase have been linked to higher mortality rates. The limited availability of effective antibiotics contributes to the severity of these infections, impacting patient outcomes and posing a direct threat to public health.
- Extended Hospital Stays:
- Infections associated with Klebsiella pneumoniae carbapenemase often result in prolonged hospital stays for affected individuals. The challenges in managing and treating these infections contribute to extended recovery times, placing an additional burden on healthcare resources.
- Resource Strain:
- The presence of Klebsiella pneumoniae carbapenemase strains healthcare resources. The need for isolation protocols, increased surveillance, and specialized care for infected individuals strain both personnel and financial resources, affecting the overall capacity of healthcare systems.
- Impact on Vulnerable Populations:
- Vulnerable populations, such as those with compromised immune systems or underlying health conditions, are particularly susceptible to the impact of Klebsiella pneumoniae carbapenemase. The limited treatment options and increased severity of infections pose heightened risks for these individuals.
- Transmission Challenges:
- The ease with which Klebsiella pneumoniae carbapenemase can be transmitted within healthcare settings poses a formidable challenge. Controlling the spread of the bacterium requires heightened infection prevention measures and close monitoring to prevent outbreaks.
- Need for Specialized Interventions:
- Managing infections involving Klebsiella pneumoniae carbapenemase necessitates specialized interventions. The complexity of treatment and the potential for resistance development highlight the need for tailored approaches and a focus on developing new strategies to combat this emerging threat.
- Global Public Health Concern:
- The global spread of KPC transforms it into a significant public health concern. The interconnectedness of healthcare systems worldwide underscores the importance of international collaboration to effectively address the impact of Klebsiella pneumoniae carbapenemase on a broader scale.
Strategies and Management:
Effectively managing Klebsiella pneumoniae carbapenemase (KPC) requires a multifaceted approach, recognizing the complexity of antibiotic resistance. Antibiotic stewardship programs play a pivotal role by optimizing the use of available antibiotics, minimizing unnecessary prescriptions, and curbing the development of resistance. In healthcare settings, robust infection prevention measures are essential to control the spread of Klebsiella pneumoniae carbapenemase. This involves stringent adherence to hand hygiene, isolation protocols for infected patients, and thorough environmental cleaning.
Research and development efforts are crucial for identifying alternative treatment options and developing new antibiotics to stay ahead of bacterial evolution. International collaboration enhances the collective response to KPC, allowing the exchange of information, experiences, and best practices. As we navigate the challenges posed by KPC, a comprehensive strategy encompassing antibiotic stewardship, infection prevention, research, and global collaboration becomes imperative to effectively manage this emerging threat in healthcare settings.
- Antibiotic Stewardship:
- Antibiotic stewardship programs have gained prominence as a crucial strategy in managing KPC. These initiatives focus on optimizing antibiotic use, preventing unnecessary prescriptions, and minimizing the development of antibiotic resistance.
- Infection Prevention Measures:
- Robust infection prevention measures are vital in curbing the spread of KPC. This includes strict adherence to hand hygiene, isolation protocols for infected patients, and environmental cleaning to reduce the risk of transmission within healthcare settings.
- Research and Development:
- Ongoing research into alternative treatment options and the development of new antibiotics are essential components in the battle against KPC. The urgency to address antibiotic resistance underscores the need for innovative solutions to stay ahead of evolving bacterial threats.
- International Collaboration:
-
- Given the global nature of KPC, international collaboration is paramount. Sharing information, experiences, and best practices enables a more coordinated response to tackle this emerging threat collectively.
Points strategies and management:
- Antibiotic Stewardship Programs:
- Implementing and strengthening antibiotic stewardship programs to optimize the use of available antibiotics, curbing unnecessary prescriptions and minimizing the risk of resistance development.
- Infection Prevention Measures:
- Rigorous adherence to infection prevention measures, including strict hand hygiene, isolation protocols for infected individuals, and thorough environmental cleaning to prevent the spread of Klebsiella pneumoniae carbapenemase (KPC) within healthcare settings.
- Research for Alternative Treatments:
- Investing in research and development to identify alternative treatment options and novel antibiotics, addressing the challenge of KPC and staying ahead of bacterial resistance.
- International Collaboration:
- Fostering international collaboration for the exchange of information, experiences, and best practices. A collective effort enhances the global response to KPC, recognizing its widespread impact.
- Surveillance and Monitoring:
- Implementing robust surveillance and monitoring systems to track the prevalence of KPC, identify outbreaks, and inform timely interventions to prevent further spread.
- Education and Training:
- Providing education and training for healthcare professionals on the identification, prevention, and management of KPC. Enhancing awareness contributes to effective response strategies.
- Public Health Initiatives:
- Engaging in public health initiatives to raise awareness among the general population about the importance of antibiotic stewardship, infection prevention, and the collective effort needed to combat KPC.
- Adaptive Policies:
- Developing adaptive policies that address the evolving nature of antibiotic resistance, allowing healthcare systems to respond effectively to emerging challenges posed by KPC.
- Collaboration with Industry:
- Collaborating with pharmaceutical and healthcare industries to encourage the development of new antibiotics and innovative solutions to combat KPC, ensuring a diverse arsenal against resistant bacteria.
- Continuous Monitoring and Evaluation:
- Establishing systems for continuous monitoring and evaluation of implemented strategies. Regular assessments allow for adjustments and improvements in the management of KPC, aligning with evolving healthcare needs.
Conclusion:
Klebsiella pneumoniae carbapenemase poses a multifaceted challenge to healthcare systems worldwide. Understanding its origins, impact, and the strategies employed to manage its spread is crucial in navigating the complex landscape of antibiotic resistance. As the medical community grapples with evolving bacterial threats, a concerted effort towards research, infection prevention, and international collaboration becomes paramount in safeguarding the efficacy of our antibiotic arsenal and ensuring effective patient care in the face of KPC.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023