Lymphangiomatosis: Navigating the Intricacies of a Rare Disease
Introduction
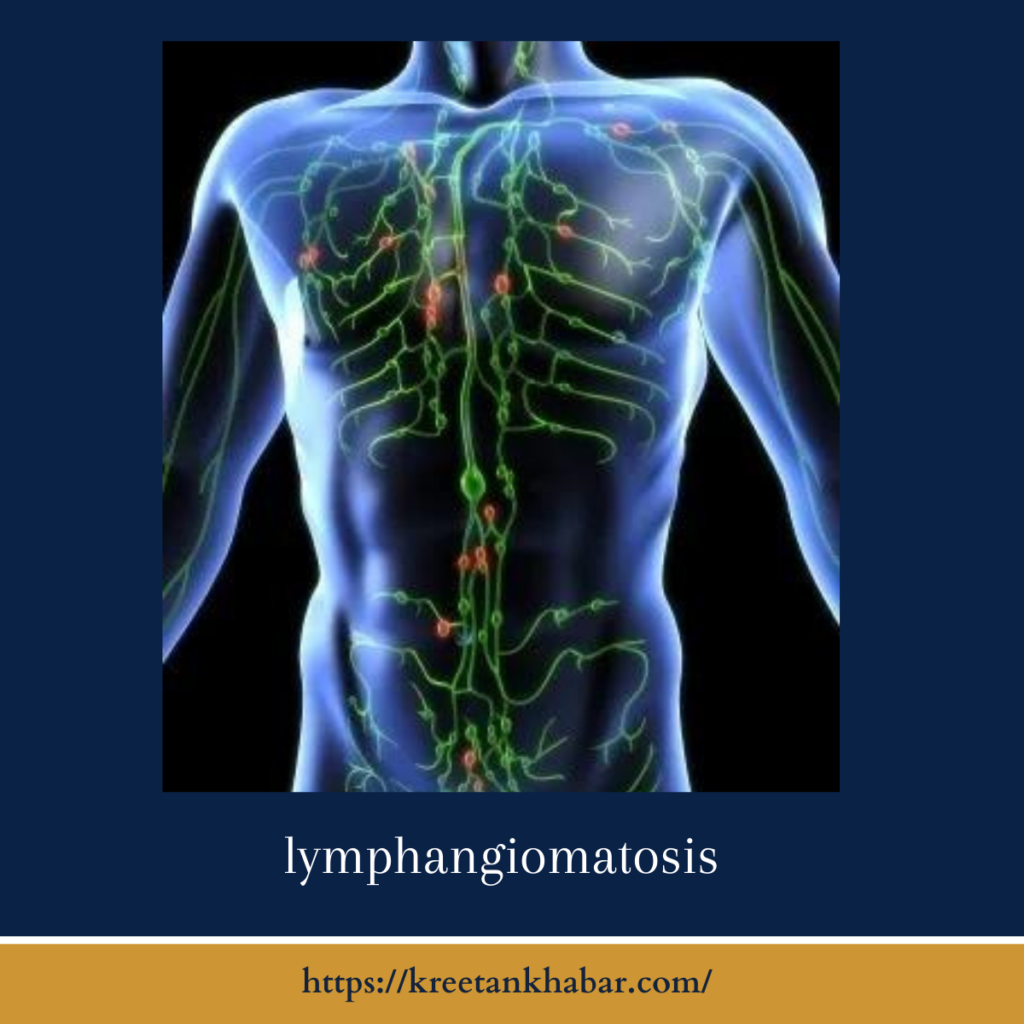
In the realm of rare diseases, lymphangiomatosis stands as a medical enigma, often challenging both patients and healthcare professionals alike. This condition, characterized by the abnormal proliferation of lymphatic vessels, can affect various parts of the body, making its diagnosis and treatment complex. In this article, we delve into the intricate world of lymphangiomatosis, exploring its causes, manifestations, diagnosis, and potential treatment options.
Understanding Lymphangiomatosis
Lymphangiomatosis, pronounced as “lim-fan-gee-uh-MAT-oh-sis,” is an uncommon disorder characterized by the formation of multiple cystic or capillary-like structures within the lymphatic system. These growths, known as lymphangiomas, can develop anywhere in the body, including the skin, soft tissues, bones, and internal organs.
Causes of Lymphangiomatosis
While the exact causes of lymphangiomatosis remain elusive, it is believed to be a congenital condition, meaning it is present at birth. Genetic mutations or abnormalities are suspected to play a role in its development. It can also occur as a result of lymphatic malformations that may become more apparent later in life.
Manifestations of Lymphangiomatosis
The symptoms and manifestations of lymphangiomatosis can vary widely based on the location and extent of the lymphangiomas. Common features may include:
- Soft Tissue Swelling: Lymphangiomas in soft tissues can lead to swelling, most often in the limbs or head and neck region.
- Pain and Discomfort: Some patients experience pain or discomfort due to the pressure caused by the cystic growths on surrounding tissues and organs.
- Respiratory Distress: In severe cases, lymphangiomas in the chest or lungs can cause respiratory difficulties, coughing, and wheezing.
- Bone Abnormalities: Lymphangiomatosis can lead to bone deformities and fractures when it affects the skeletal system.
- Complications: If lymphangiomas occur within the abdominal or thoracic cavities, they can lead to serious complications affecting vital organs.
Diagnosis of Lymphangiomatosis
The diagnosis of lymphangiomatosis often involves a combination of imaging studies and clinical assessment. These may include:
- Ultrasound: Ultrasonography is commonly used to visualize lymphangiomas in superficial tissues.
- CT and MRI Scans: Computed tomography (CT) and magnetic resonance imaging (MRI) scans provide detailed images of lymphangiomas within the body.
- Biopsy: A biopsy of the affected tissue or fluid from a lymphangioma may be performed to confirm the diagnosis.
- Genetic Testing: In some cases, genetic testing may be carried out to identify potential underlying genetic factors.
here are key points about the diagnosis of lymphangiomatosis:
1. Clinical Evaluation: The diagnosis of lymphangiomatosis typically begins with a thorough clinical evaluation. Healthcare professionals review the patient’s medical history and perform a physical examination to assess any visible symptoms or swelling.
2. Imaging Studies: Imaging plays a crucial role in diagnosing lymphangiomatosis. Various imaging techniques are used to visualize the lymphatic abnormalities, including:
- Ultrasound: Ultrasonography is often employed to assess lymphangiomas in superficial tissues, providing real-time images.
- CT (Computed Tomography): CT scans offer detailed cross-sectional images of lymphangiomas, helping to determine their size, location, and extent within the body.
- MRI (Magnetic Resonance Imaging): MRI scans provide highly detailed images and are particularly useful for assessing lymphangiomas in soft tissues and internal organs.
3. Biopsy: To confirm the diagnosis, a biopsy may be performed. This involves obtaining a sample of tissue or fluid from the lymphangioma, which is then examined under a microscope. Biopsies help identify the characteristic features of lymphangiomatosis and rule out other conditions.
4. Genetic Testing: In some cases, genetic testing may be considered, especially if there is suspicion of an underlying genetic cause. Genetic tests can help identify specific mutations or abnormalities that may contribute to the development of lymphangiomatosis.
5. Consultation with Specialists: Diagnosing and managing lymphangiomatosis often involves a multidisciplinary approach. Patients may be referred to specialists such as radiologists, pathologists, and genetic counselors to ensure a comprehensive evaluation and diagnosis.
6. Differential Diagnosis: It’s important to differentiate lymphangiomatosis from other conditions that may present with similar symptoms or imaging findings, such as lymphatic malformations, hemangiomas, or other cystic lesions.
7. Clinical Presentation: The diagnosis may also take into account the patient’s clinical presentation, including symptoms and physical findings. The location of lymphangiomas and the presence of associated complications guide the diagnostic process.
In summary, the diagnosis of lymphangiomatosis involves a combination of clinical evaluation, imaging studies, biopsies, and, in some cases, genetic testing. Accurate diagnosis is essential to tailor appropriate treatment plans and provide the best care for individuals with this rare condition.
Treatment Options
Treating lymphangiomatosis can be complex and typically depends on the extent and location of the lymphangiomas, as well as the individual patient’s needs. Treatment options may include:
- Observation: In some cases, especially when the lymphangiomas are small and asymptomatic, a “watch-and-wait” approach may be recommended.
- Surgery: Surgical removal of the lymphangiomas may be considered, although it can be challenging due to their infiltrative nature.
- Medications: Certain medications, such as sirolimus, have shown promise in reducing the size and symptoms of lymphangiomas.
- Palliative Care: For patients with advanced or inoperable disease, palliative care focuses on symptom management and improving the quality of life.
here are key points about the treatment options for lymphangiomatosis:
1. Observation and Monitoring:
- In cases where lymphangiomatosis is asymptomatic or mild, a conservative approach involving regular observation and monitoring may be recommended.
- Regular check-ups and imaging studies are used to track the progression and assess the need for intervention.
2. Surgical Intervention:
- Surgery is considered for patients with localized or accessible lymphangiomas. The goal is to remove the abnormal lymphatic tissue.
- Surgical resection may be challenging due to the infiltrative nature of lymphangiomatosis, but it can provide relief when feasible.
- Complications and risks associated with surgery, such as damage to adjacent structures, are carefully evaluated.
3. Sclerotherapy:
- Sclerotherapy involves injecting a sclerosing agent into the lymphangioma, causing it to shrink and collapse.
- This minimally invasive procedure is often used for superficial or smaller lesions and may help reduce symptoms and improve appearance.
4. Embolization:
- In cases where lymphangiomas are vascular and have significant blood flow, embolization can be employed.
- A catheter is used to block the blood vessels supplying the lymphangioma, leading to its reduction in size.
5. Medications:
- Medications like sirolimus, which is an mTOR inhibitor, have shown promise in treating lymphangiomatosis. They can help reduce the size and symptoms of lymphangiomas, especially in cases where surgery is not feasible or effective.
6. Supportive Care:
- For patients with advanced or inoperable lymphangiomatosis, supportive care focuses on managing symptoms and improving the patient’s quality of life.
- This may involve pain management, physiotherapy, and addressing complications caused by lymphangiomas.
7. Multidisciplinary Care:
- Lymphangiomatosis often requires a multidisciplinary approach involving specialists in radiology, surgery, oncology, and genetics, among others.
- A team of experts collaborates to determine the most appropriate treatment strategy for each patient.
8. Genetic Counseling:
- In cases where a genetic basis for lymphangiomatosis is suspected, genetic counseling may be offered to affected individuals and their families to assess the risk of recurrence in future generations.
9. Research and Clinical Trials:
- Ongoing research and clinical trials are exploring novel treatment options and therapeutic approaches for lymphangiomatosis.
- Patients may have the opportunity to participate in these trials to access cutting-edge treatments.
10. Long-Term Follow-Up: – Long-term follow-up care is essential for patients with lymphangiomatosis, as the condition can be recurrent. – Regular check-ups and imaging studies help monitor for disease progression or complications.
In summary, the treatment of lymphangiomatosis is individualized, considering factors like the extent and location of lymphangiomas, symptoms, and the overall health of the patient. The chosen approach may involve observation, surgery, minimally invasive procedures, medications, and supportive care, often with input from a multidisciplinary team of specialists.
Conclusion
Lymphangiomatosis, with its intricate web of symptoms and challenging diagnosis, is a condition that warrants specialized medical attention and care. Understanding its causes, manifestations, and treatment options is essential for patients, their families, and healthcare providers as they navigate the complexities of this rare disease. Ongoing research and advancements in treatment options offer hope for improved management and outcomes for those living with lymphangiomatosis.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023