Meningioma: Causes, Symptoms, Diagnosis, and Treatment
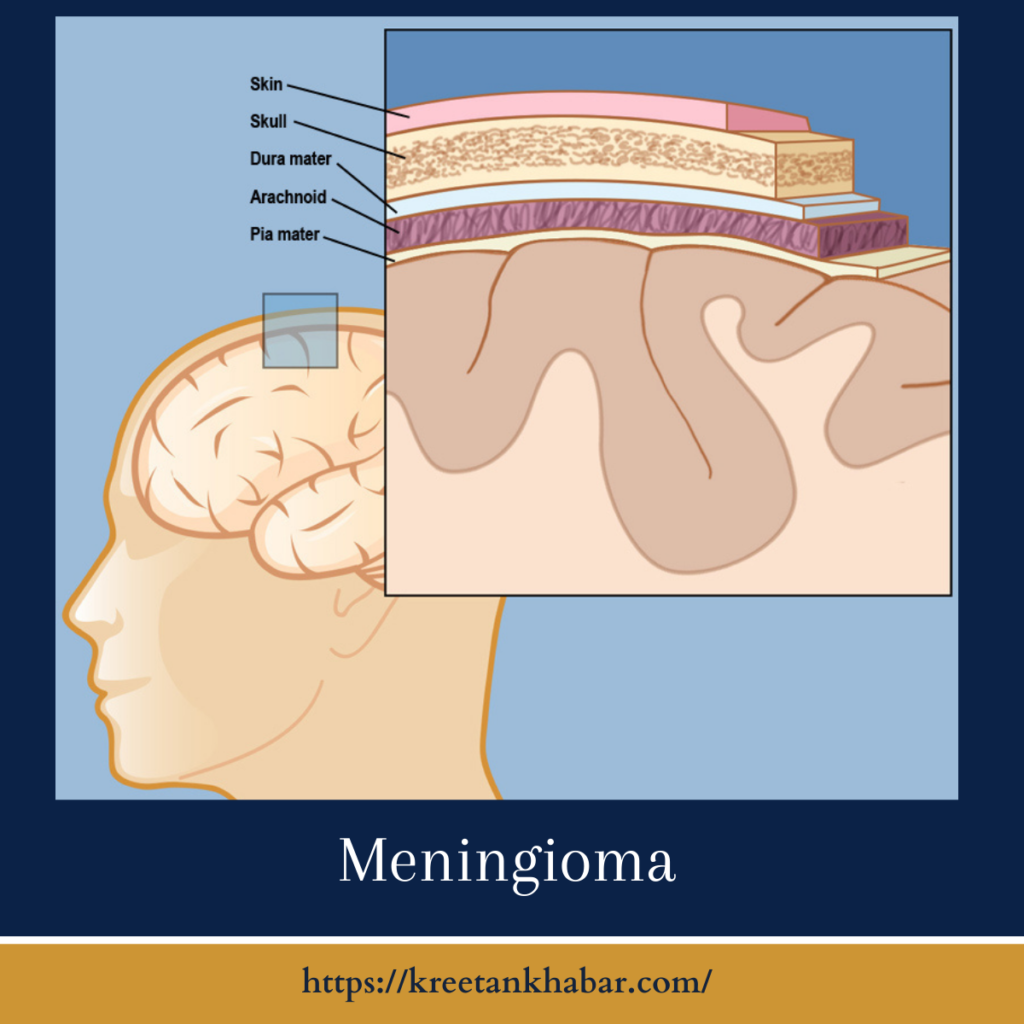
Meningiomas (also known as meningeal tumor) are tumors that develop in the meninges, the layers of tissue covering the brain and spinal cord. While most meningeal tumor are noncancerous (benign), they can still impact neurological function and quality of life. In this article, we will delve into the key aspects of meningeal tumor, exploring their causes, symptoms, diagnostic approaches, and available treatment options.
Causes of Meningioma:
- Cellular Origin: Meningiomas arise from the meninges, specifically from arachnoid cap cells. The exact trigger for the development of these tumors is not fully understood.
- Genetic Factors: Some meningiomas may be associated with genetic conditions such as neurofibromatosis type 2 (NF2) or familial meningioma, suggesting a hereditary component.
- Hormonal Influence: There is evidence to suggest that hormonal factors, particularly the hormone progesterone, may play a role in the growth of meningeal tumor, as they often express progesterone receptors.
- Radiation Exposure: Previous exposure to ionizing radiation, especially during childhood, is considered a risk factor for the development of meningeal tumor.
Symptoms of Meningioma:
- Headaches: Persistent and worsening headaches are a common symptom. They may be dull or throbbing and often occur in the morning.
- Seizures: Meningiomas can irritate the brain, leading to seizures. The type and severity of seizures can vary.
- Visual Disturbances: Tumors near the optic nerve can cause visual symptoms, such as blurred vision, double vision, or a loss of vision.
- Weakness or Numbness: Depending on the location of the tumor, weakness or numbness in the limbs may occur.
- Changes in Personality or Behavior: meningeal tumor impacting specific areas of the brain can result in alterations in personality, mood swings, or changes in behavior.
- Cognitive Impairment: Memory problems, difficulty concentrating, and other cognitive deficits may arise.
- Loss of Smell: Tumors near the olfactory nerve can lead to a loss of sense of smell.
- Difficulty Speaking or Swallowing: meningeal tumor affecting the areas of the brain responsible for speech and swallowing can cause difficulties in these functions.
Diagnosis of Meningioma:
- Neurological Examination: A thorough neurological examination is conducted to assess reflexes, coordination, and sensory functions.
- Imaging Studies: Magnetic Resonance Imaging (MRI) is the primary imaging modality for visualizing meningeal tumor and determining their location, size, and relationship to surrounding structures.
- Computerized Tomography (CT) Scan: CT scans may be used to provide additional information, especially regarding the bone structures.
- Biopsy (in Some Cases): While most meningeal tumor can be diagnosed through imaging studies, a biopsy may be recommended in certain situations to confirm the diagnosis and assess the tumor’s grade.
- Cerebral Angiography: This procedure involves injecting a contrast dye into blood vessels to evaluate blood flow and detect abnormalities in the blood vessels near the tumor.
Diagnosis of Meningioma: Key Points
- Clinical Evaluation: The diagnostic process begins with a thorough clinical evaluation by a healthcare professional, including a detailed medical history and a comprehensive neurological examination.
- Symptom Assessment: Identification and analysis of symptoms such as persistent headaches, seizures, visual disturbances, weakness, or changes in behavior play a crucial role in suspecting meningioma.
- Imaging Studies (MRI and CT Scan):
- MRI (Magnetic Resonance Imaging): This is the primary imaging modality for diagnosing meningiomas. It provides detailed images of the brain, highlighting the location, size, and characteristics of the tumor.
- CT (Computed Tomography) Scan: CT scans may be used to complement MRI, especially for assessing bony structures and detecting calcifications.
- Biopsy (if needed): While imaging studies can often confirm the presence of a meningioma, a biopsy may be recommended in certain cases to determine the tumor’s grade and confirm the diagnosis. However, due to the risk associated with brain biopsy, it is usually reserved for specific situations.
- Cerebral Angiography: In some cases, cerebral angiography may be performed to assess blood flow in the surrounding vessels and evaluate the tumor’s relationship with the vascular structures.
- Review of Imaging Characteristics: Radiologists analyze the imaging characteristics of the meningioma, including its shape, borders, enhancement pattern, and any signs of compression or invasion of adjacent structures.
- Consideration of Hormone Receptor Status: For meningiomas expressing hormone receptors, particularly progesterone receptors, the assessment of hormone receptor status may influence treatment decisions.
- Collaboration with Specialists: Neurosurgeons, neurologists, and neuroradiologists often collaborate in the diagnostic process, bringing their expertise to interpret imaging findings and recommend further assessments or interventions.
- Evaluation of Patient History and Risk Factors: Understanding the patient’s medical history, including any previous radiation exposure or family history of meningiomas, is essential for a comprehensive diagnosis.
- Differential Diagnosis: Differentiating meningiomas from other brain tumors or conditions that present with similar symptoms is a critical aspect of the diagnostic process.
- Monitoring and Follow-Up: In cases where the meningioma is not causing immediate symptoms, regular monitoring through follow-up imaging studies may be recommended to track any changes in size or characteristics.
- Patient Communication and Informed Consent: Clear communication with the patient regarding the diagnostic process, potential procedures, and the need for informed consent is integral to fostering understanding and collaboration.
- Confirmation of Diagnosis: The culmination of clinical evaluation, imaging studies, and, if necessary, biopsy results leads to the confirmation of the meningioma diagnosis.
- Grade Classification (if applicable): If a biopsy is performed, the meningioma may be classified into different grades based on its histological characteristics, influencing treatment decisions and prognosis.
- Multidisciplinary Approach: The diagnosis and subsequent management of meningioma often involve a multidisciplinary team, including neurosurgeons, oncologists, radiation therapists, and other specialists, ensuring a comprehensive and well-coordinated approach.
In summary, the diagnosis of meningioma is a multifaceted process that combines clinical evaluation, advanced imaging studies, and, when necessary, biopsy results. A collaborative effort among healthcare professionals and effective communication with the patient contribute to a thorough understanding of the condition, facilitating timely and appropriate treatment decisions.
Treatment Options for Meningioma:
- Observation: Small, slow-growing meningeal tumor that are not causing significant symptoms may be monitored through regular imaging studies without immediate intervention.
- Surgery: Surgical removal of the meningioma is often the primary treatment, especially if the tumor is causing symptoms, growing rapidly, or if there is concern about its location.
- Radiation Therapy: In cases where complete surgical removal is challenging, radiation therapy may be employed to target and shrink the tumor.
- Hormone Therapy: Some meningeal tumor with progesterone receptors may respond to hormone therapy, although its efficacy is still under investigation.
- Medication for Symptom Management: Medications may be prescribed to manage symptoms such as seizures, headaches, or swelling.
Prognosis and Outlook:
The prognosis for meningioma varies based on factors such as the tumor’s size, location, and grade. The majority of meningeal tumor are benign and have a favorable prognosis, especially when treated promptly. However, the recurrence rate can vary, and regular follow-up with imaging studies is often recommended.
Conclusion
Meningiomas are complex tumors that require a multidisciplinary approach for accurate diagnosis and effective management. Advances in imaging technology, surgical techniques, and targeted therapies continue to enhance the options available for individuals affected by meningeal tumor. Seeking prompt medical attention for persistent or worsening neurological symptoms is crucial for early diagnosis and optimal outcomes.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023