Pelvic Organ Prolapse: When the Body’s Support System Weakens
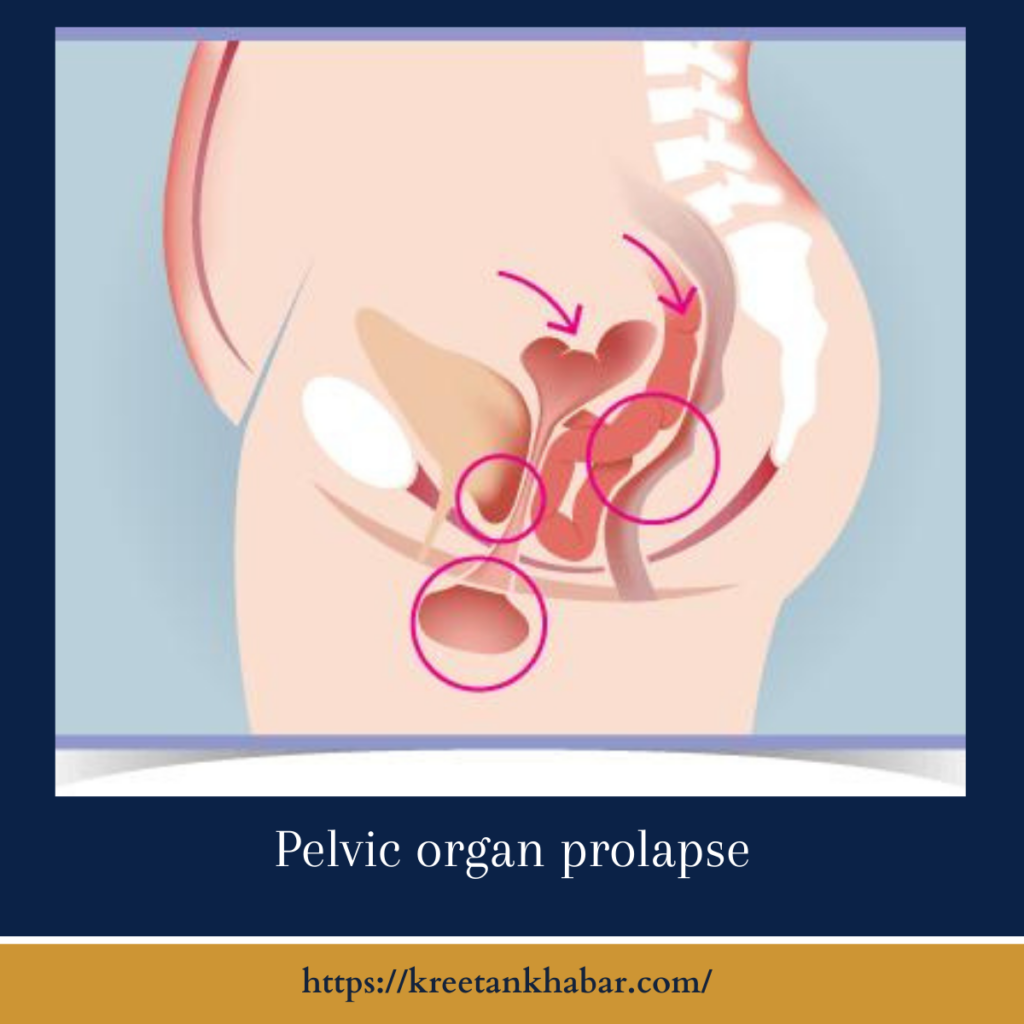
Pelvic organ prolapse (POP) is a common but often underdiscussed medical condition that affects many women, particularly as they age. It occurs when the muscles and tissues that support the pelvic organs weaken, causing one or more of these organs to shift or descend into the vaginal canal. In this article, we will explore pelvic organ prolapse, its causes, symptoms, diagnosis, and treatment options.
Causes of Pelvic Organ Prolapse:
Several factors can contribute to the development of pelvic organ prolapse:
- Pregnancy and Childbirth: The process of pregnancy and vaginal childbirth can strain and weaken the pelvic floor muscles and tissues, increasing the risk of POP, especially in women who have had multiple pregnancies.
- Aging: As women age, hormonal changes can lead to decreased muscle and tissue elasticity, which may weaken the pelvic floor.
- Chronic Constipation and Straining: Frequent constipation and straining during bowel movements can stress the pelvic floor, potentially leading to prolapse.
- Obesity: Excess weight can put additional pressure on the pelvic area, contributing to POP.
- Genetic Factors: Some individuals may have a genetic predisposition to pelvic organ prolapse.
- Hysterectomy: Surgical removal of the uterus (hysterectomy) can alter pelvic support and increase the risk of prolapse.
here are key points about the causes of Pelvic Organ Prolapse (POP):
Causes of Pelvic Organ Prolapse:
- Pregnancy and Childbirth: The process of pregnancy and vaginal childbirth is one of the most common causes of POP. During pregnancy, the weight of the growing fetus places strain on the pelvic floor muscles and supporting tissues. Vaginal childbirth, especially when accompanied by prolonged labor, the use of forceps, or multiple pregnancies, can further weaken these structures, increasing the risk of prolapse.
- Aging: As women age, hormonal changes, particularly the decrease in estrogen levels during menopause, can lead to reduced muscle and tissue elasticity in the pelvic region. This natural aging process can contribute to the weakening of the pelvic floor and increase the likelihood of prolapse.
- Chronic Constipation and Straining: Frequent and sustained straining during bowel movements, often associated with chronic constipation, can stress the pelvic floor muscles and connective tissues. Over time, this strain may weaken these structures, making them more susceptible to prolapse.
- Obesity: Excess body weight places additional pressure on the pelvic area, including the pelvic floor. The increased strain can lead to the weakening of these supportive structures and raise the risk of developing POP.
- Genetic Factors: Some individuals may have a genetic predisposition to pelvic organ prolapse. Family history can be a contributing factor, although the specific genetic mechanisms are not fully understood.
- Hysterectomy: Surgical removal of the uterus (hysterectomy) is a common procedure that can alter the natural support system of the pelvis. Depending on the surgical approach and techniques used, hysterectomy may increase the risk of pelvic organ prolapse.
- Chronic Coughing: Conditions associated with chronic coughing, such as chronic obstructive pulmonary disease (COPD) or long-term smoking, can lead to increased intra-abdominal pressure. This pressure can strain the pelvic floor muscles and tissues, potentially contributing to prolapse.
- Connective Tissue Disorders: Some connective tissue disorders, such as Ehlers-Danlos syndrome and Marfan syndrome, can affect the strength and integrity of the pelvic floor support structures, increasing the risk of prolapse.
- Heavy Lifting: Frequent heavy lifting, especially when performed incorrectly or without proper support, can strain the pelvic area and weaken the pelvic floor muscles.
It’s important to note that pelvic organ prolapse is a multifactorial condition, often influenced by a combination of these factors. Additionally, not all individuals with these risk factors will develop POP, and some cases of POP occur without any identifiable cause.
Symptoms of Pelvic Organ Prolapse:
The symptoms of POP can vary in severity and may include:
- Pelvic Pressure: A sensation of fullness or pressure in the pelvis, often described as feeling like something is falling out.
- Vaginal Bulge: A noticeable bulge or protrusion in the vaginal canal, which may become more pronounced with standing, coughing, or straining.
- Discomfort or Pain: Pelvic pain, discomfort, or aching, especially during intercourse or prolonged standing.
- Urinary Symptoms: Frequent urination, urgency, incontinence, or difficulty emptying the bladder completely.
- Bowel Symptoms: Constipation, difficulty with bowel movements, or fecal incontinence.
- Sexual Dysfunction: Pain or discomfort during sexual intercourse due to the change in pelvic anatomy.
Diagnosis of Pelvic Organ Prolapse:
Diagnosing POP typically involves a combination of medical history, physical examination, and, in some cases, imaging studies. Key steps in the diagnostic process may include:
- Medical History: Detailed discussions about symptoms, medical history, and relevant factors like pregnancies and childbirth.
- Pelvic Examination: A thorough physical examination, often performed while the patient is lying down and straining, to assess the extent and type of prolapse.
- Pelvic Ultrasound or MRI: In some cases, imaging studies like pelvic ultrasound or magnetic resonance imaging (MRI) may be used to visualize the pelvic organs and confirm the diagnosis.
Treatment Options for Pelvic Organ Prolapse:
The treatment of pelvic organ prolapse depends on the severity of symptoms, the type of prolapse, and the individual’s overall health. Treatment options include:
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles through exercises can help improve mild to moderate prolapse and alleviate some symptoms.
- Pessaries: These are removable devices that can be inserted into the vagina to support the pelvic organs and reduce symptoms.
- Physical Therapy: Pelvic floor physical therapy, including biofeedback and electrical stimulation, can be effective in strengthening and improving muscle tone in the pelvic area.
- Hormone Therapy: In some cases, hormone replacement therapy may be considered to address symptoms related to hormonal changes, particularly in postmenopausal women.
- Surgery: Surgical intervention may be necessary for severe cases of POP. Procedures may involve repairing or reinforcing the pelvic floor, removing the prolapsed tissue, or performing a hysterectomy with or without additional repairs.
The choice of treatment should be tailored to the individual’s specific needs and circumstances. It is essential for women experiencing symptoms of pelvic organ prolapse to seek medical evaluation and discuss treatment options with a healthcare provider. With appropriate care, many women can find relief from the discomfort and inconvenience of POP and improve their quality of life.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023