Polycystic Kidney Disease: A Closer Look at Causes, Symptoms, and Hope for the Future
Introduction:
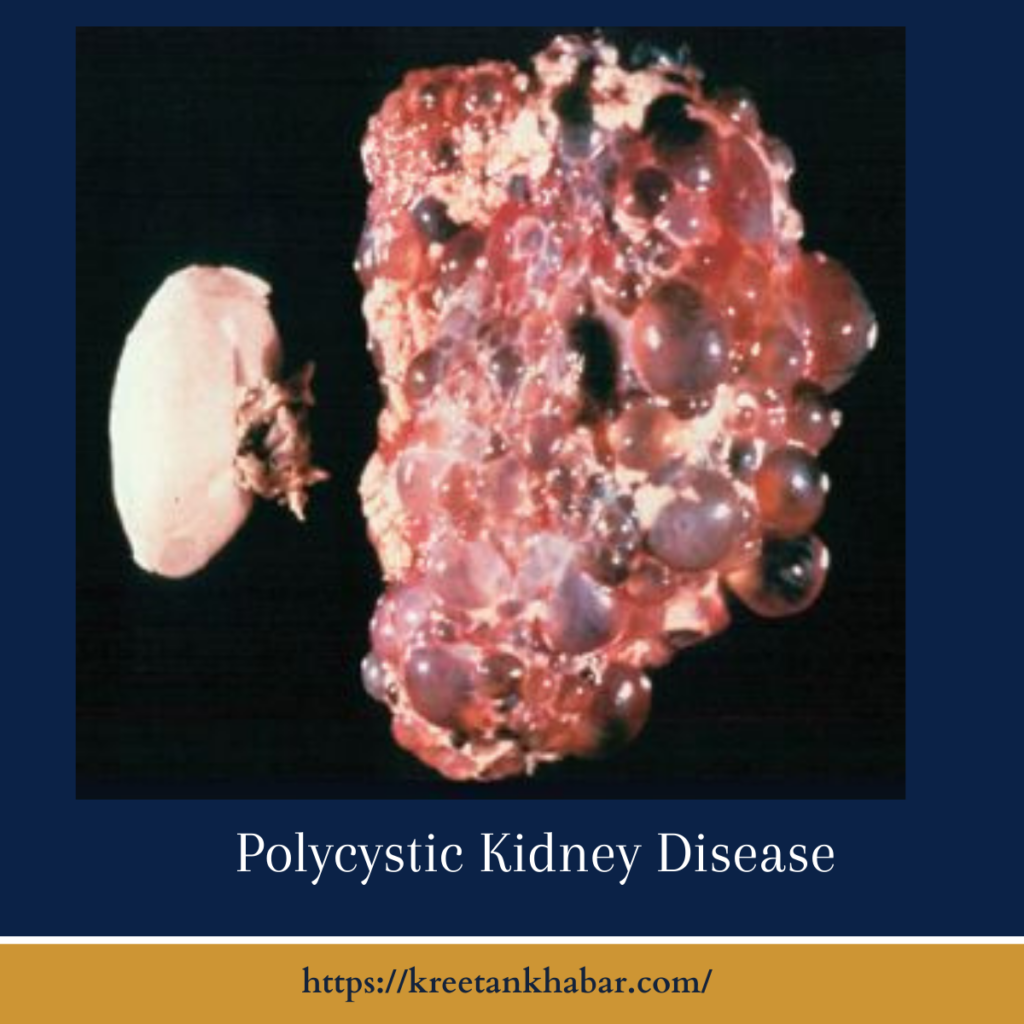
Polycystic Kidney Disease (PKD) stands as an intricate puzzle within the realm of renal disorders, affecting millions worldwide. Characterized by the formation of fluid-filled cysts on the kidneys, PKD can lead to a range of complications and challenges for those affected. In this exploration, we delve into the complexities of PKD, shedding light on its causes, symptoms, and the promising avenues of research that offer hope for the future.
Understanding Polycystic Kidney Disease:
Polycystic Kidney Disease, often hereditary, comes in two primary forms: Autosomal Dominant Polycystic Kidney Disease (ADPKD) and Autosomal Recessive Polycystic Kidney Disease (ARPKD). ADPKD is the more prevalent form, typically surfacing in adulthood, while ARPKD is usually diagnosed in infancy or early childhood.
Causes:
Genetics play a pivotal role in the development of PKD. Mutations in specific genes, such as PKD1 and PKD2, are implicated in ADPKD, disrupting the normal functioning of proteins involved in maintaining kidney structure. ARPKD, on the other hand, stems from mutations in the PKHD1 gene, impacting kidney and liver development.
- Genetic Culprit:
- Polycystic Kidney Disease (PKD) is predominantly a result of genetic mutations. In particular, mutations in the PKD1 and PKD2 genes are associated with Autosomal Dominant Polycystic Kidney Disease (ADPKD), while mutations in the PKHD1 gene contribute to Autosomal Recessive Polycystic Kidney Disease (ARPKD).
- Autosomal Dominant Inheritance:
- ADPKD follows an autosomal dominant pattern, meaning that an affected individual has a 50% chance of passing the mutated gene to each of their children. This form of inheritance explains why PKD often runs in families.
- Protein Aberrations:
- The PKD1 and PKD2 genes encode for proteins involved in maintaining the structure and function of kidney cells. Mutations in these genes lead to abnormal proteins, disrupting the delicate balance necessary for proper kidney development and function.
- Autosomal Recessive Dynamics:
- In contrast, ARPKD is inherited in an autosomal recessive manner. Both parents must carry a copy of the mutated gene for a child to develop ARPKD. This recessive inheritance pattern often results in the disease manifesting in early childhood.
- Impact on Kidney and Liver Development:
- The PKHD1 gene associated with ARPKD is crucial for normal kidney and liver development. Mutations in this gene disrupt the delicate processes involved in organ formation, contributing to the cystic changes observed in affected individuals.
- Genetic Diversity:
- The wide spectrum of mutations and genetic diversity within affected families explains the variability in the severity and onset of PKD symptoms. Even among individuals sharing the same genetic mutation, the disease can manifest differently.
- Sporadic Cases:
- While PKD is primarily genetic, sporadic cases where individuals develop the condition without a family history do occur. These cases may involve de novo mutations, which spontaneously arise in an individual rather than being inherited from parents.
- Second-Hit Hypothesis:
- The “second-hit” hypothesis suggests that, in ADPKD, an additional genetic event or environmental factor may be required to trigger the formation of cysts. This concept adds a layer of complexity to our understanding of PKD development.
- Research Frontiers:
- Ongoing research is focused on identifying additional genetic and environmental factors that may influence the course of PKD. Unraveling these complexities could provide valuable insights into potential therapeutic targets and interventions.
- Personalized Medicine Prospects:
- As genetic research advances, there is growing optimism for personalized medicine approaches. Tailoring treatments based on an individual’s specific genetic profile holds promise for more effective and targeted management of Polycystic Kidney Disease.
Symptoms:
The symptoms of PKD can vary widely, even within families. Abdominal pain, high blood pressure, and blood in the urine are common indicators. As cysts grow, they can lead to kidney enlargement, compromising their function and potentially resulting in kidney failure. Recognizing these signs early is crucial for effective management and intervention.
- Silent Onset:
- Polycystic Kidney Disease (PKD) often starts its journey silently, with no noticeable symptoms in the early stages. This subtle onset can make detection challenging until the cysts grow large enough to cause complications.
- Abdominal Pain and Discomfort:
- As cysts enlarge, they exert pressure on the surrounding kidney tissue, leading to persistent abdominal pain and discomfort. The pain may range from dull and nagging to sharp and intense, depending on the size and location of the cysts.
- Hypertension (High Blood Pressure):
- PKD has a notorious connection with hypertension. The presence of cysts can disrupt the normal blood flow in the kidneys, triggering an increase in blood pressure. Controlling hypertension is crucial in managing PKD and preventing further kidney damage.
- Hematuria (Blood in Urine):
- The development of cysts can cause bleeding within the kidneys, leading to hematuria or blood in the urine. While not always visible, microscopic traces of blood may be detected in urine tests.
- Urinary Tract Infections (UTIs):
- The structural changes in the kidneys due to cyst formation create an environment conducive to urinary tract infections. Recurrent UTIs can be a common symptom of PKD.
- Kidney Enlargement:
- As cysts multiply and grow, the kidneys themselves undergo enlargement. This physical expansion can sometimes be felt by healthcare professionals during a physical examination.
- Renal Impairment:
- Progressive cyst growth can lead to a decline in kidney function. Impaired renal function may manifest as symptoms like fatigue, weakness, and a decrease in urine output.
- Intracranial Aneurysms:
- In some cases, PKD is associated with the development of intracranial aneurysms—bulging and weakened areas in blood vessels within the brain. Rupture of these aneurysms can result in a severe medical emergency.
- Valley Sign:
- The “valley sign” refers to the visual appearance of cysts on imaging studies. Cysts often create a characteristic appearance resembling a valley, aiding in the diagnosis of PKD.
- Varied Onset and Severity:
- Symptoms of PKD can vary widely among individuals, even within the same family. The age of onset, the rate of cyst growth, and the severity of symptoms are influenced by factors such as genetic variations and environmental influences.
- Extrarenal Manifestations:
- Beyond the kidneys, PKD can have extrarenal manifestations. For example, cysts may develop in the liver and other organs, contributing to a range of associated symptoms.
- Psychosocial Impact:
- Living with PKD extends beyond the physical symptoms. The chronic nature of the disease, coupled with the uncertainty it brings, can have a profound impact on mental health and well-being.
Understanding and recognizing these symptoms early on are crucial for timely intervention, effective management, and improved quality of life for individuals dealing with Polycystic Kidney Disease.
Challenges and Complications:
Living with PKD poses numerous challenges. The progressive nature of the disease, coupled with the potential for kidney failure, necessitates a multidisciplinary approach to care. Managing complications such as hypertension, urinary tract infections, and cyst-related pain becomes integral to maintaining a reasonable quality of life for those with PKD.
Hope on the Horizon:
Despite the intricate nature of PKD, the landscape of research offers promising developments. Ongoing studies delve into potential therapies aimed at slowing cyst growth and preserving kidney function. Genetic therapies and precision medicine hold particular promise, offering tailored approaches based on an individual’s unique genetic makeup.
Clinical trials exploring novel medications and interventions are underway, offering a glimmer of hope for a future where PKD may be more effectively managed or even cured. The collaborative efforts of researchers, healthcare professionals, and advocacy groups are driving progress, ushering in a new era of understanding and treatment for PKD.
Conclusion:
Polycystic Kidney Disease is a formidable adversary, impacting the lives of individuals and their families. Yet, amidst the challenges, there is reason for hope. Advances in genetics, targeted therapies, and a deeper understanding of the disease’s intricacies paint a promising picture for the future. As the medical community continues to unravel the mysteries of PKD, there is an unwavering commitment to improving the lives of those affected and moving closer to a world where Polycystic Kidney Disease is no longer an insurmountable obstacle.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023