Posterior Tibial Tendon Dysfunction: A Comprehensive Guide
Introduction:
Our bodies are intricate systems of tendons, ligaments, and bones working together to support our every move. When one component falters, it can disrupt the delicate balance, leading to various complications. One such concern is Posterior Tibial Tendon Dysfunction (PTTD), a condition that often goes unnoticed until it significantly impacts our daily lives. In this article, we will explore the intricacies of PTTD, its causes, symptoms, and potential treatments.
Understanding Posterior Tibial Tendon Dysfunction:
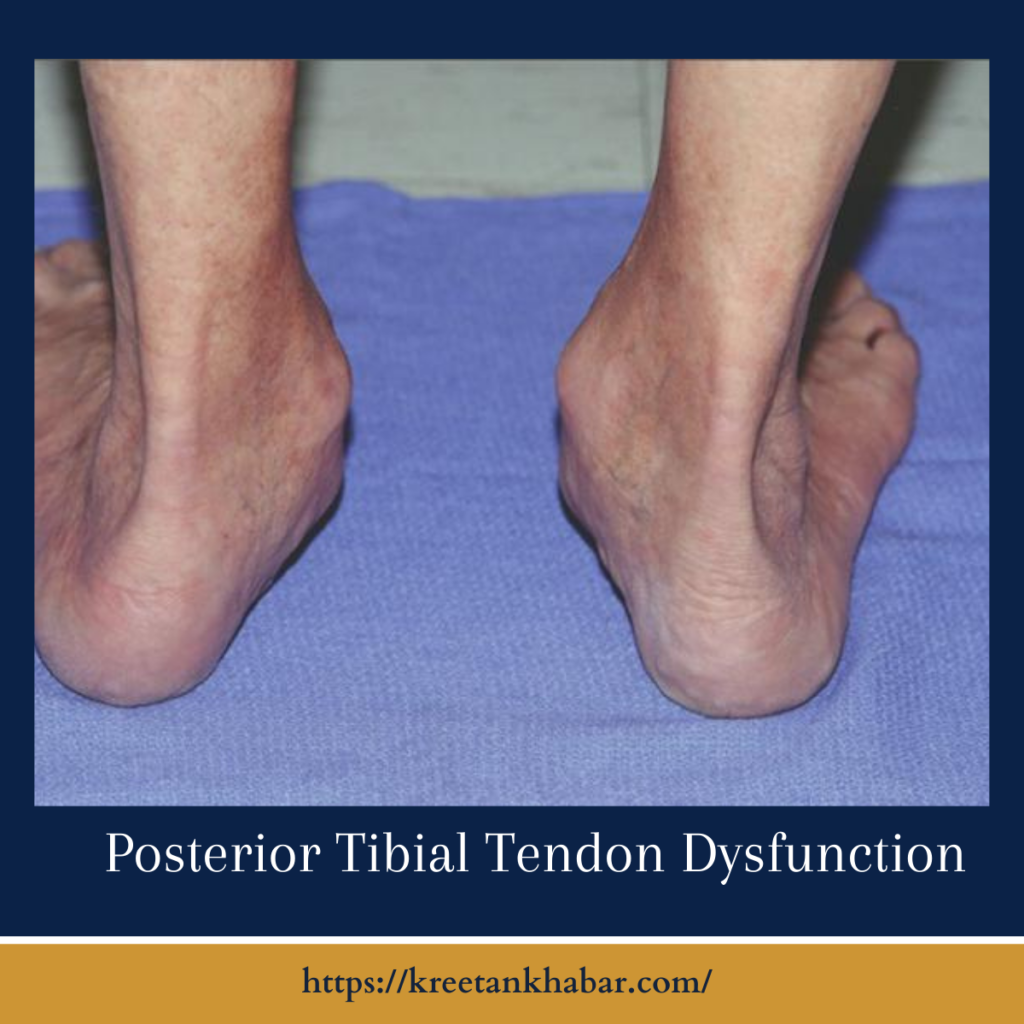
Posterior Tibial Tendon Dysfunction is a condition affecting the posterior tibial tendon, a crucial structure that supports the arch of the foot. This tendon plays a pivotal role in maintaining the foot’s stability during activities like walking, running, and standing. When the tendon becomes weakened or damaged, it can no longer provide the necessary support, leading to a collapse of the arch and subsequent foot deformities.
Causes of PTTD:
Several factors contribute to the development of Posterior Tibial Tendon Dysfunction . One primary cause is overuse or repetitive strain on the posterior tibial tendon, often associated with activities that involve excessive walking or running. Additionally, obesity, genetics, and inflammatory conditions like rheumatoid arthritis can increase the risk of developing this dysfunction. Understanding these factors is crucial for early detection and effective management.
- Overuse and Repetitive Strain:
- PTTD often stems from overworking the posterior tibial tendon, commonly associated with activities that put excessive strain on the foot. Long periods of walking, running, or standing can lead to wear and tear, gradually weakening the tendon over time.
- Obesity and Excess Weight:
- Carrying excess body weight places increased stress on the posterior tibial tendon, contributing to its degeneration. Maintaining a healthy weight is crucial in preventing unnecessary strain on this vital foot structure.
- Genetic Predisposition:
- Genetics play a role in the development of Posterior Tibial Tendon Dysfunction . Individuals with a family history of flat feet or other foot-related conditions may have a higher susceptibility to this dysfunction. Understanding familial predispositions can aid in early detection and preventive measures.
- Age-Related Changes:
- As we age, our tendons naturally undergo changes, becoming less elastic and more prone to degeneration. The aging process can compromise the structural integrity of the posterior tibial tendon, making older individuals more susceptible to Posterior Tibial Tendon Dysfunction .
- Inflammatory Conditions:
- Inflammatory disorders such as rheumatoid arthritis can contribute to the development of Posterior Tibial Tendon Dysfunction . The inflammation weakens the tendon, compromising its ability to support the arch of the foot and leading to the dysfunction.
- Trauma or Injury:
- Direct trauma or injury to the foot, ankle, or lower leg can damage the posterior tibial tendon. This damage may occur suddenly or develop over time, particularly if the injury is not properly addressed or allowed to heal.
- Improper Footwear:
- Wearing shoes that lack proper arch support or fail to distribute weight evenly can contribute to Posterior Tibial Tendon Dysfunction . High heels and shoes with inadequate stability may exacerbate the strain on the posterior tibial tendon, increasing the risk of dysfunction.
- Systemic Diseases:
- Certain systemic diseases, such as diabetes, can affect the health of tendons and contribute to Posterior Tibial Tendon Dysfunction . Individuals with pre-existing medical conditions should be vigilant about foot health and discuss any concerns with their healthcare providers.
- Biomechanical Abnormalities:
- Irregularities in foot structure or gait abnormalities can place undue stress on the posterior tibial tendon. Understanding one’s biomechanics and addressing any abnormalities through orthotic devices or physical therapy can be crucial in preventing dysfunction.
- Ignoring Early Warning Signs:
- Neglecting the early symptoms of Posterior Tibial Tendon Dysfunction , such as pain, swelling, or a flattening of the foot arch, can allow the condition to progress. Early intervention is key in managing and preventing the worsening of posterior tibial tendon dysfunction.
Symptoms:
Recognizing the symptoms of Posterior Tibial Tendon Dysfunction is essential for prompt intervention. Early stages may manifest as pain, swelling, or a gradual flattening of the foot arch. As the dysfunction progresses, individuals may experience difficulty standing on their toes, inward rolling of the ankle, and an altered gait. Ignoring these signs can lead to further complications, such as arthritis and deformities.
Diagnosis:
Diagnosing Posterior Tibial Tendon Dysfunction requires a thorough examination by a healthcare professional. They may perform physical tests, review medical history, and order imaging studies like X-rays or MRI scans to assess the extent of tendon damage. Early diagnosis facilitates better outcomes, as it allows for timely intervention and the implementation of appropriate treatment plans.
- Clinical Evaluation:
- Diagnosis of Posterior Tibial Tendon Dysfunction (PTTD) often begins with a thorough clinical examination. Healthcare professionals will assess the patient’s medical history, inquire about symptoms, and conduct physical tests to evaluate the range of motion, strength, and stability of the affected foot and ankle.
- Gait Analysis:
- Observing the patient’s gait can provide valuable insights into the extent of Posterior Tibial Tendon Dysfunction . Changes in walking patterns, such as an inward roll of the ankle or an altered stride, may indicate dysfunction in the posterior tibial tendon.
- Imaging Studies:
- X-rays are commonly employed to rule out other potential causes of foot pain and deformities. Magnetic Resonance Imaging (MRI) or ultrasound may be recommended to visualize the soft tissues, including the posterior tibial tendon, and assess the severity of damage.
- Tendon Function Tests:
- Specialized tests, such as the single-limb heel rise test, may be performed to evaluate the strength and function of the posterior tibial tendon. Difficulty in rising onto the toes or instability during the test can be indicative of PTTD.
- Comparison with the Unaffected Side:
- A comparative analysis of the affected foot with the unaffected side aids in highlighting any asymmetry or abnormalities. This side-to-side comparison helps clinicians gauge the degree of tendon dysfunction and its impact on foot structure.
- Pain Mapping:
- Patients often report pain in specific areas of the foot or ankle. Pain mapping, where individuals identify and describe the location and nature of pain, assists healthcare providers in pinpointing the affected areas and contributing factors.
- Dynamic Assessments:
- Dynamic assessments involve evaluating the foot and ankle in motion. Healthcare professionals may observe the patient walking, standing on tiptoes, or performing other weight-bearing activities to better understand the dynamic nature of PTTD.
- Functional Ankle Instability Tests:
- Since PTTD can contribute to ankle instability, specific tests may be conducted to assess the overall stability of the ankle joint. This includes evaluating the response of the foot and ankle to stress and various movements.
- Blood Tests:
- In cases where inflammatory conditions are suspected, blood tests may be conducted to check for markers of inflammation. This can help identify underlying systemic factors contributing to PTTD.
- Collaborative Approach:
- Diagnosing PTTD often involves collaboration between orthopedic specialists, podiatrists, and physical therapists. A comprehensive and interdisciplinary approach ensures a thorough assessment and a well-rounded understanding of the patient’s condition, facilitating effective treatment planning.
Remember, early diagnosis is crucial for successful management of Posterior Tibial Tendon Dysfunction. If you experience persistent foot pain or notice changes in your gait, consult a healthcare professional for a comprehensive evaluation.
Treatment Options:
The management of PTTD often involves a multifaceted approach tailored to the severity of the condition. Conservative measures may include rest, ice, compression, and elevation (RICE), along with physical therapy to strengthen the supporting muscles. Orthotic devices and supportive footwear can aid in alleviating pressure on the affected tendon.
In more advanced cases, where conservative methods prove insufficient, surgical intervention may be considered. Surgical options range from tendon repair to joint fusion, depending on the extent of damage and the individual’s overall health.
Prevention and Lifestyle Modifications:
Prevention is always preferable to treatment. Adopting a proactive approach involves maintaining a healthy weight, incorporating strength and flexibility exercises into your routine, and choosing appropriate footwear. Regular check-ups with a healthcare professional can help identify and address potential issues before they escalate.
Conclusion:
Posterior Tibial Tendon Dysfunction is a complex condition that requires careful attention and timely intervention. Understanding the causes, recognizing the symptoms, and pursuing appropriate treatment options can significantly improve outcomes. By prioritizing foot health and taking proactive measures, individuals can stride confidently towards a future free from the constraints of PTTD.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023