Posterior Vaginal Wall Prolapse
Introduction:
In the intricate landscape of women’s health, there are conditions that often linger in the shadows, one of which is posterior vaginal wall prolapse. This unspoken concern, though less discussed, can significantly impact a woman’s quality of life. In this article, we’ll delve into the intricacies of posterior vaginal wall prolapse, exploring its causes, symptoms, and the avenues of support and treatment available to those affected.
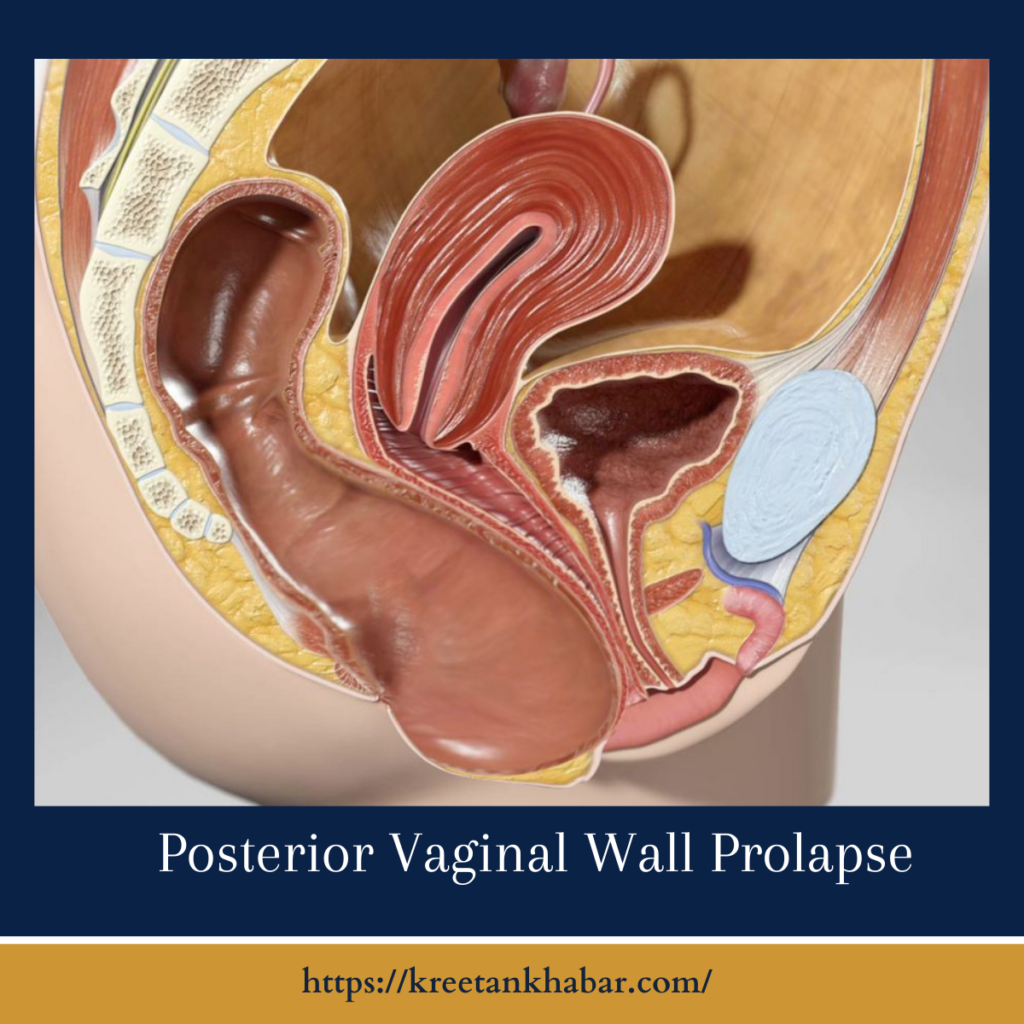
Unraveling the Basics:
Posterior vaginal wall prolapse, also known as rectocele, is a condition where the thin wall of tissue that separates the rectum from the vagina weakens, allowing the rectum to bulge into the vaginal space. This can lead to a range of symptoms that may include discomfort, difficulty with bowel movements, and a sense of pelvic pressure.
Common Causes:
Understanding the factors that contribute to posterior vaginal wall prolapse is essential. Childbirth, especially multiple vaginal deliveries, can weaken the pelvic floor muscles and supportive tissues. Other risk factors include aging, hormonal changes, and chronic conditions that strain the pelvic region, such as chronic constipation.
- Childbirth Trauma: The physical toll of childbirth, especially multiple vaginal deliveries, is a primary contributor to posterior vaginal wall prolapse. The stretching and weakening of pelvic floor muscles and tissues during labor and delivery can compromise the structural support of the vaginal wall.
- Aging and Hormonal Changes: As women age, hormonal changes, particularly the decline in estrogen levels during menopause, can lead to a reduction in the elasticity and strength of pelvic tissues. This hormonal shift contributes to the weakening of the supportive structures, increasing the risk of posterior vaginal wall prolapse.
- Chronic Constipation: Conditions that lead to chronic constipation play a significant role in the development of posterior vaginal wall prolapse. Straining during bowel movements over an extended period can strain the pelvic floor muscles, leading to weakening and increased vulnerability.
- Genetic Predisposition: While not a direct cause, a genetic predisposition to connective tissue disorders or inherent weaknesses in pelvic floor support structures can contribute to an increased susceptibility to posterior vaginal wall prolapse.
- Pelvic Floor Muscle Weakness: Weakness in the pelvic floor muscles, whether due to genetic factors, aging, or a sedentary lifestyle, can compromise the ability of these muscles to provide adequate support to the pelvic organs, contributing to prolapse.
- Obesity and Excess Weight: Excess weight and obesity place additional stress on the pelvic floor and can contribute to the development or exacerbation of posterior vaginal wall prolapse. Maintaining a healthy weight is crucial in preventing and managing this condition.
- Connective Tissue Disorders: Certain connective tissue disorders, such as Ehlers-Danlos syndrome or Marfan syndrome, can affect the strength and integrity of tissues throughout the body, including those supporting the pelvic organs. Individuals with these conditions may be at a higher risk of prolapse.
- Repeated Heavy Lifting: Jobs or activities that involve repeated heavy lifting can strain the pelvic floor muscles and contribute to the development of posterior vaginal wall prolapse. Proper lifting techniques and avoiding excessive strain are essential in preventing this condition.
- Pelvic Surgery or Trauma: Previous pelvic surgeries or traumatic injuries to the pelvic region can disrupt the normal anatomy and weaken the supportive structures, increasing the risk of prolapse.
- Chronic Coughing: Persistent, chronic coughing due to conditions such as chronic obstructive pulmonary disease (COPD) or long-term smoking can create repetitive stress on the pelvic floor muscles, potentially contributing to the development of posterior vaginal wall prolapse.
Understanding the diverse factors that can lead to posterior vaginal wall prolapse is crucial for both prevention and effective management. Identifying and addressing these underlying causes can guide tailored interventions and contribute to better outcomes for individuals affected by this condition.
Recognizing the Signs:
Posterior vaginal wall prolapse often manifests with distinct signs that should not be ignored. Women may experience a bulging sensation in the vagina, discomfort during sexual intercourse, or difficulty fully emptying the bowels. These symptoms, while sensitive, are crucial indicators that warrant attention and prompt consultation with a healthcare professional.
The Impact on Quality of Life:
The repercussions of posterior vaginal wall prolapse extend beyond the physical realm. Emotional and psychological well-being can be profoundly affected, as women may grapple with feelings of self-consciousness, embarrassment, or a perceived loss of femininity. Understanding the holistic impact of this condition emphasizes the importance of seeking support and treatment.
Exploring Treatment Options:
Fortunately, there are avenues of support and treatment available for those navigating posterior vaginal wall prolapse. Conservative measures, such as pelvic floor exercises and lifestyle modifications, may offer relief for mild cases. For more severe instances, surgical interventions, ranging from minimally invasive procedures to traditional repairs, can provide long-term solutions.
Embracing Open Dialogue:
Breaking the silence surrounding posterior vaginal wall prolapse is a vital step toward empowerment. Open dialogue between healthcare providers and patients is essential, fostering an environment where women feel comfortable discussing their symptoms, seeking guidance, and exploring treatment options. This shared understanding is a cornerstone for effective care.
Pelvic Health and Lifestyle:
In addition to medical interventions, incorporating pelvic health practices into daily life can make a substantial difference. Maintaining a healthy weight, avoiding constipation through dietary measures, and practicing pelvic floor exercises can contribute to overall pelvic health and potentially prevent the progression of posterior vaginal wall prolapse.
Support Networks and Education:
Support networks and educational resources play a pivotal role in the journey of those affected by posterior vaginal wall prolapse. Women can find solace and guidance through support groups, where shared experiences foster understanding and resilience. Education about the condition, its causes, and available treatments empowers individuals to make informed decisions about their health.
Conclusion:
Posterior vaginal wall prolapse may be an unspoken concern, but it is not one that should be endured in silence. By shedding light on the intricacies of this condition, we hope to encourage women to prioritize their pelvic health, seek support when needed, and embark on a journey of empowerment and well-being. Through understanding, dialogue, and comprehensive care, we can navigate the complexities of posterior vaginal wall prolapse with compassion and resilience.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023