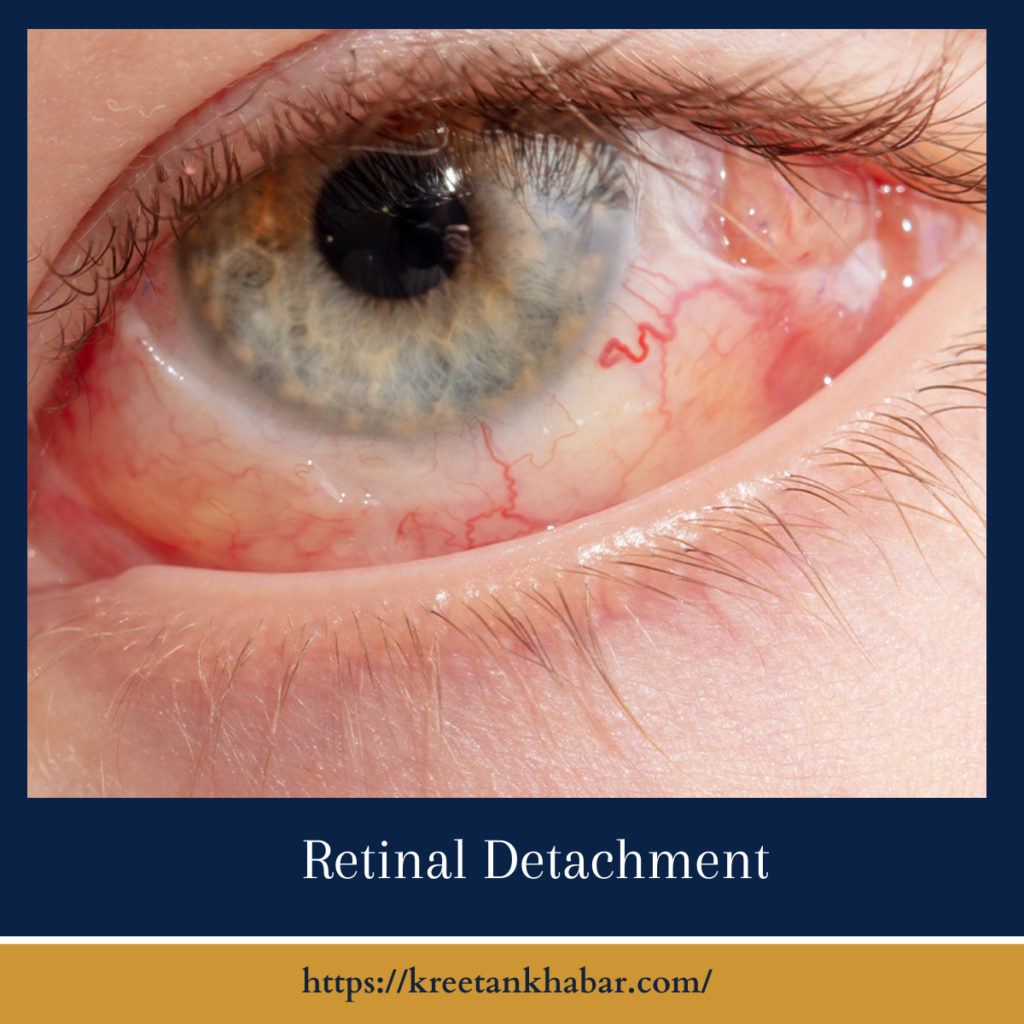
Retinal Detachment
Introduction:
In the delicate realm of vision, where light weaves the tapestry of our world, the threat of retinal detachment lurks like a shadow in the periphery. A silent intruder, it whispers of sudden darkness, blurred edges, and the fragility of sight. Join us on a journey through the maze of Retinal Detachment, exploring its nuances, symptoms, and the quest for restoration that unfolds within the intricate folds of the eye.
The Symphony of Sight:
Before we delve into the realm of Retinal Detachment, let’s acquaint ourselves with the symphony that is the human eye. The retina, a thin layer of tissue lining the back of the eye, captures the visual narrative and translates it into the language of nerves, guiding the images that dance in our minds.
Understanding Retinal Detachment:
The Unseen Culprit: Retinal detachment occurs when the retina peels away from the underlying layers of the eye. This detachment can be caused by various factors, with tears or breaks in the retina’s delicate fabric allowing fluid to seep in and create a separation.
Types of Retinal Detachment: There are three primary types of retinal detachment – rhegmatogenous, tractional, and exudative. Rhegmatogenous detachment, resulting from retinal tears, is the most common, while tractional detachment involves scar tissue, and exudative detachment is caused by fluid accumulation.
Symptoms – The Ominous Whispers: Retinal detachment doesn’t announce its arrival with a flourish; rather, it whispers ominous signs. These may include sudden flashes of light, the appearance of floaters, and a shadow or curtain descending over the visual field. Immediate attention is crucial when these symptoms arise.
- Flashes of Light: One of the earliest and often unsettling symptoms of retinal detachment is the sudden appearance of flashes of light. These flashes may resemble lightning streaks or twinkling stars and are a signal that the retina might be under stress.
- Floaters and Spots: Small, dark specks or floaters drifting across the visual field can indicate the detachment of the retina. These seemingly innocuous spots, when noticed suddenly and persistently, should prompt immediate attention.
- Shadow or Curtain Descending: A noticeable shadow or curtain-like effect descending over the visual field is a hallmark symptom of retinal detachment. This occurrence signifies that a portion of the retina has detached, causing a disruption in the normal visual perception.
- Blurred or Reduced Vision: As the detachment progresses, vision becomes compromised, leading to blurred or reduced visual acuity. Individuals may experience a sudden decline in their ability to see clearly, as if a veil has been cast over their eyes.
- Loss of Peripheral Vision: Retinal detachment often affects peripheral vision first. Individuals may notice a gradual or sudden loss of side vision, creating a tunnel-like effect and restricting the overall field of view.
- Sensation of a “Cobweb” or “Hairnet”: Some people describe the sensation of a cobweb or hairnet obstructing their vision. This feeling is attributed to the physical displacement of the detached retina, causing an irregularity in the visual experience.
- Distorted Vision (Metamorphopsia): Metamorphopsia, or the distortion of shapes and straight lines, is another symptom associated with retinal detachment. Objects may appear warped or misshapen, indicating a disruption in the normal alignment of the retina.
- Sudden Onset: Unlike gradual changes in vision, retinal detachment often presents with a sudden onset of symptoms. Individuals may be going about their day when they suddenly notice these visual disturbances, prompting the need for immediate attention.
- Painless Nature: One notable aspect of retinal detachment is its generally painless nature. Unlike conditions like eye infections or injuries, individuals with retinal detachment may not experience significant discomfort, making the symptoms easy to overlook.
- Association with Trauma or High Myopia: While retinal detachment can occur spontaneously, it is more common in individuals with a history of eye trauma or those with high degrees of nearsightedness (myopia). Understanding personal risk factors can help individuals recognize the importance of promptly addressing any unusual visual symptoms.
Recognizing these symptoms as potential indicators of retinal detachment is crucial for seeking immediate medical attention. Early diagnosis and intervention significantly enhance the chances of successful treatment and preserving vision.
Risk Factors: Factors that increase the risk of retinal detachment include aging, a history of eye surgeries, severe nearsightedness, and a family history of retinal detachment. Trauma to the eye, diabetes, and inflammatory eye disorders can also contribute to the vulnerability of the retina.
Diagnosis – Peering into the Depths: Diagnosing retinal detachment involves a meticulous eye examination. Imaging techniques such as ultrasound and optical coherence tomography (OCT) offer a deeper look into the layers of the eye, aiding in the identification and classification of detachment.
- Comprehensive Eye Examination: Diagnosis of retinal detachment begins with a thorough eye examination conducted by an eye care professional. This examination includes an assessment of visual acuity, intraocular pressure, and a detailed examination of the retina using specialized instruments.
- Dilated Pupil Examination: Dilation of the pupil allows for a more comprehensive view of the retina. By enlarging the pupil, the eye care professional gains a clearer view of the back of the eye and can identify any abnormalities or signs of detachment.
- Visual Field Testing: Visual field testing assesses the entire scope of an individual’s vision, including peripheral vision. This test helps in identifying any deficits or irregularities in the visual field that may be indicative of retinal detachment.
- Ultrasound Imaging: In cases where direct visualization of the retina is challenging, ultrasound imaging can be employed. This non-invasive technique uses sound waves to create an image of the eye’s interior, helping to detect the presence and extent of retinal detachment.
- Optical Coherence Tomography (OCT): Optical Coherence Tomography is a high-resolution imaging test that provides detailed cross-sectional images of the retina. It is particularly useful in detecting macular detachment and assessing the layers of the retina with precision.
- Fluorescein Angiography: Fluorescein angiography involves injecting a dye into the bloodstream, which then highlights the blood vessels in the retina. By capturing images of the dye’s flow, this diagnostic tool helps identify any areas of leakage or abnormalities in blood circulation.
- Differentiating from Other Eye Conditions: Diagnosing retinal detachment involves differentiating it from other eye conditions with similar symptoms, such as vitreous detachment or macular degeneration. A careful consideration of medical history and symptoms aids in accurate diagnosis.
- Assessment of Risk Factors: Understanding and assessing individual risk factors, such as a history of eye trauma, high myopia, or a family history of retinal detachment, are crucial components of the diagnostic process. These factors contribute to the overall evaluation of the patient’s eye health.
- Timely Intervention: Given the urgency associated with retinal detachment, prompt diagnosis is essential. Any sudden onset of visual disturbances or symptoms should be immediately reported to an eye care professional for a swift and accurate assessment.
- Collaboration with Retina Specialists: In complex cases or cases requiring surgical intervention, collaboration with retina specialists becomes integral. Retina specialists are experts in the intricate surgical procedures involved in reattaching the retina and restoring optimal visual function.
The diagnosis of retinal detachment relies on a combination of clinical expertise, advanced imaging technologies, and a proactive approach to reporting and addressing symptoms. Early detection and intervention remain paramount in preserving vision and mitigating the potential complications associated with this sight-threatening condition.
Treatment – Stitching the Fabric: The urgency of treating retinal detachment is paramount. Surgical interventions, such as scleral buckling or vitrectomy, aim to reattach the retina and prevent further vision loss. The choice of procedure depends on the type and severity of the detachment.
Post-Operative Care: Recovery from retinal detachment surgery involves a delicate dance of healing. Positioning restrictions, meticulous care, and regular follow-ups are essential to monitor the reattachment process and ensure the best possible visual outcome.
Emotional Landscape: Beyond the physical ramifications, retinal detachment can cast shadows on the emotional landscape. Adapting to changes in vision, navigating the uncertainties of recovery, and embracing the support of loved ones become integral aspects of the human experience with this condition.
Conclusion:
Retinal Detachment, with its silent entry and profound impact, beckons us to unravel the intricacies of our vision’s vulnerability. As we navigate the shadows and embark on the journey of diagnosis, treatment, and recovery, knowledge becomes our guiding light. It is a testament to the resilience of the human spirit, the strides of medical science, and the enduring quest to preserve the kaleidoscope of sight. In this exploration, we discover not just the fragility of the retina but the strength woven into the very fabric of our vision.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023