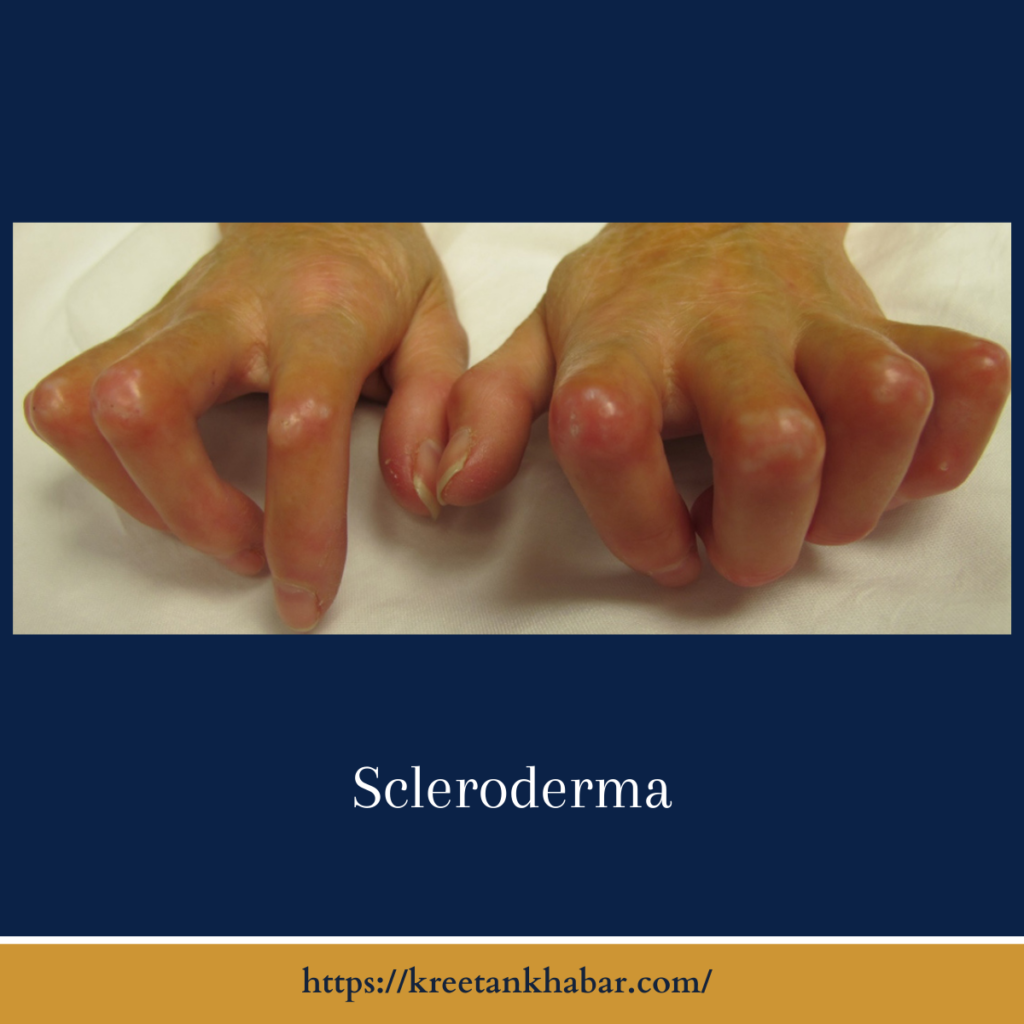
Scleroderma
Introduction:
In the intricate landscape of autoimmune disorders, one condition stands out as both mystifying and complex – Scleroderma(also known as thickening). This rare and often enigmatic disease affects the connective tissues of the body, leaving an indelible mark on those who navigate its challenges. In this exploration, we embark on a journey into the world of Scleroderma, unraveling its mysteries, understanding its impact, and shedding light on the resilience of those who face its unique complexities.
The Canvas of Scleroderma:
Scleroderma, derived from the Greek words “skleros” (hard) and “derma” (skin), manifests as an overproduction of collagen – the protein that provides structure to the skin and internal organs. This overproduction leads to the characteristic thickening and hardening of tissues, affecting various parts of the body.
The Faces of Scleroderma:
Scleroderma is a multifaceted condition with diverse presentations, falling into two main categories: localized and systemic. Localized thickening primarily impacts the skin, while systemic scleroderma extends its reach to internal organs, such as the lungs, heart, kidneys, and digestive tract. Within these broad categories, different subtypes further delineate the complexities of this condition.
Understanding the Symptomatic Palette:
The symptoms of thickening are as varied as the individuals it affects. From the tightening and thickening of the skin to the potential involvement of vital organs, the symptomatic palette of thickening is vast. Raynaud’s phenomenon, a condition where small blood vessels constrict in response to cold or stress, is often an early sign. Skin changes, joint pain, digestive issues, and respiratory problems are among the myriad manifestations, making scleroderma a truly intricate puzzle for both patients and healthcare professionals.
The Enigma of Scleroderma’s Cause:
While the precise cause of thickening remains elusive, it is widely recognized as an autoimmune disorder. The immune system, designed to protect the body, goes awry and mistakenly attacks healthy tissues. Genetic predisposition, environmental factors, and immune system dysfunction are believed to contribute to the development of scleroderma, yet the interplay of these elements remains a subject of ongoing research.
- Autoimmune Origins: thickening cause lies in the intricate realm of autoimmune dysfunction. The immune system, typically tasked with safeguarding the body, misfires and targets its own healthy tissues. In the case of thickening, this immune system confusion leads to excessive production of collagen, triggering the characteristic hardening and thickening of tissues.
- Genetic Predisposition: A genetic component adds complexity to the thickening puzzle. While not directly inherited, there appears to be a genetic predisposition that influences an individual’s susceptibility to autoimmune disorders. Specific genetic markers and variations are being explored to better understand the hereditary aspects of scleroderma.
- Environmental Triggers: Environmental factors are thought to contribute to the development of thickening, acting as triggers in genetically predisposed individuals. These triggers may include exposure to certain toxins, infections, or other external influences that, when combined with a genetic susceptibility, set the stage for the onset of scleroderma.
- Immune System Aberrations: Dysfunction within the immune system is a central theme in the cause of thickening. The immune system’s inability to distinguish between foreign invaders and healthy tissues results in an inflammatory response. This chronic inflammation, coupled with an overactive production of collagen, contributes to the characteristic symptoms of the disease.
- Vascular Abnormalities: thickening often involves abnormalities in the vascular system. Blood vessels can be damaged, leading to reduced blood flow and contributing to complications such as Raynaud’s phenomenon, where small blood vessels constrict excessively in response to cold or stress.
- Role of Fibroblasts: Fibroblasts, cells responsible for producing collagen, play a pivotal role in the pathogenesis of thickening. In individuals with scleroderma, these cells become overactive, producing excess collagen that accumulates in the skin and internal organs. Understanding the regulation of fibroblast activity is a key focus in unraveling the cause of scleroderma.
- Association with Other Autoimmune Conditions: thickening is often associated with other autoimmune conditions, forming a complex web of interconnected disorders. The presence of specific antibodies and shared immune system aberrations further emphasizes the intricate relationship between different autoimmune conditions and provides clues to the underlying causes of scleroderma.
- Microbiome Influence: The role of the microbiome, the collection of microorganisms residing in the human body, is gaining attention in autoimmune research. Changes in the microbiome composition may influence the immune system’s behavior, and researchers are exploring the potential connection between microbiome alterations and the development of scleroderma.
- Hormonal Factors: Hormonal influences, particularly the role of estrogen, are being investigated in relation to thickening. The disease is more prevalent in women, suggesting a potential hormonal link. Understanding how hormonal factors contribute to the dysregulation of the immune system may provide insights into the cause of scleroderma.
- Ongoing Research: The cause of thickening remains an active area of research. Ongoing studies are delving into the intricate interplay of genetic, environmental, and immune system factors to unravel the mysteries surrounding this complex autoimmune disorder. As scientific understanding advances, new insights into the cause of scleroderma may pave the way for more targeted treatments and improved management strategies.
Diagnosis: A Complex Puzzle:
Diagnosing scleroderma requires a meticulous approach, often involving a combination of clinical assessments, laboratory tests, and imaging studies. Skin biopsies may be performed to examine affected tissues, while blood tests can help identify specific antibodies associated with scleroderma. The complexity of the diagnostic process underscores the need for a multidisciplinary approach, with rheumatologists, dermatologists, and other specialists collaborating to piece together the puzzle.
Navigating Life with Scleroderma:
Living with scleroderma demands resilience, adaptability, and a robust support system. The impact on daily life can be profound, ranging from challenges in mobility to adjustments in personal and professional spheres. Fatigue, pain, and emotional distress are common companions on this journey, necessitating a holistic approach to care that addresses not only physical symptoms but also the emotional and social aspects of living with a chronic condition.
Treatment and Management:
While there is no cure for scleroderma, advancements in medical research have led to improved treatment options. Medications that modulate the immune system, alleviate symptoms, and manage complications are part of the therapeutic arsenal. Physical therapy, tailored exercise regimens, and lifestyle modifications also play a crucial role in enhancing quality of life for individuals with scleroderma.
- Multidisciplinary Approach: Scleroderma demands a holistic and multidisciplinary approach to treatment. A collaborative effort involving rheumatologists, dermatologists, pulmonologists, and other specialists is essential to address the diverse range of symptoms and complications associated with the disease.
- Medications to Modulate the Immune System: Immunomodulatory medications form a crucial component of scleroderma treatment. These drugs aim to regulate the immune system, mitigate inflammation, and slow down the progression of the disease. Commonly prescribed medications include corticosteroids, disease-modifying anti-rheumatic drugs (DMARDs), and immunosuppressants.
- Symptom-Specific Medications: Tailoring medications to alleviate specific symptoms is a key aspect of scleroderma management. For example, medications targeting blood pressure and vasodilators may be prescribed to address complications like Raynaud’s phenomenon, while pain management strategies help individuals cope with discomfort.
- Physical and Occupational Therapy: Physical and occupational therapy play pivotal roles in managing scleroderma-related symptoms. These therapies focus on maintaining joint flexibility, improving mobility, and addressing muscle weakness. Customized exercise regimens enhance overall physical well-being and help individuals adapt to lifestyle changes.
- Lifestyle Modifications: Lifestyle adjustments are integral to scleroderma management. Individuals are encouraged to prioritize a balanced diet, maintain regular exercise, and manage stress. Adequate hydration and protection from extreme temperatures contribute to overall well-being and help minimize symptom exacerbations.
- Pulmonary Rehabilitation: Given the potential impact of scleroderma on the lungs, pulmonary rehabilitation is often recommended. This specialized program includes exercises, breathing techniques, and education to optimize lung function and enhance respiratory endurance.
- Treatment of Gastrointestinal Complications: Gastrointestinal complications are common in thickening, affecting the esophagus and digestive tract. Medications to address acid reflux, dietary modifications, and lifestyle changes may be recommended to manage these issues and improve overall digestive health.
- Digital Ulcer Care: Digital ulcers, a manifestation of vascular involvement in thickening, require specialized care. Wound care, medications to improve blood flow, and strategies to prevent infection are crucial components of managing digital ulcers.
- Ongoing Monitoring and Adjustments: Scleroderma is a dynamic condition, and treatment plans often require ongoing monitoring and adjustments. Regular check-ups with healthcare providers allow for the evaluation of disease progression, the assessment of treatment efficacy, and the timely modification of therapeutic strategies.
- Patient Education and Empowerment: Patient education is empowering in the management of thickening. Understanding the disease, its potential complications, and proactive self-care measures contribute to a sense of control. Patient advocacy groups and support networks play crucial roles in providing information and fostering a community of shared experiences.
- Clinical Trials and Research Participation: Participation in clinical trials and research initiatives is an active area of involvement for individuals with scleroderma. Access to experimental treatments and contributing to the advancement of scientific understanding are opportunities for those motivated to be at the forefront of scleroderma research.
- Psychosocial Support: The emotional and psychological aspects of living with scleroderma are integral to overall well-being. Psychosocial support, including counseling, support groups, and mental health resources, helps individuals navigate the emotional challenges associated with the disease and fosters resilience in the face of adversity.
- Advanced Therapies for Severe Cases: In severe cases of scleroderma, where organ involvement is significant, advanced therapies such as stem cell transplantation may be considered. These interventions, while reserved for specific circumstances, represent ongoing efforts to explore innovative approaches to scleroderma treatment.
Scleroderma management is a dynamic and individualized journey, with treatment plans tailored to address the unique needs and challenges of each individual. As research continues to advance, the landscape of scleroderma treatment holds the promise of more effective interventions and improved outcomes for those affected by this complex autoimmune disorder.
The Importance of Advocacy and Support:
The scleroderma community, both online and offline, plays a pivotal role in advocacy, awareness, and mutual support. Organizations and patient groups work tirelessly to elevate the visibility of scleroderma, promote research initiatives, and provide a lifeline of understanding for those navigating the challenges of this complex condition.
Conclusion:
Scleroderma, with its intricate tapestry of symptoms and its impact on every facet of life, remains a compelling enigma in the realm of autoimmune disorders. Yet, within this complexity lies a resilient community of individuals, healthcare professionals, and advocates dedicated to unraveling its mysteries, improving diagnostics and treatment, and offering unwavering support to those affected. As we continue to delve into the world of scleroderma, we not only uncover the complexities of the condition but also celebrate the strength, courage, and determination of those who face its challenges head-on.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023