Spinal Epidural Abscess
Introduction
Within the intricate confines of the spine, a silent threat occasionally lurks, disrupting the delicate balance of this central pillar of our musculoskeletal system. A spinal epidural abscess, though rare, unfolds as a medical enigma, requiring keen awareness and timely intervention. In this exploration, we navigate through the shadows of this stealthy intruder, delving into its origins, clinical manifestations, diagnostic intricacies, and the imperative journey of treatment.
The Anatomy of Spinal Epidural Abscess
A spinal epidural abscess is a localized collection of pus within the epidural space, the outermost layer of the spinal canal. This insidious formation may compress the spinal cord or nerve roots, leading to a cascade of symptoms and potential complications. The origins of this abscess are diverse, often stemming from bacterial or fungal infections that find their way into the epidural space.
Clinical Manifestations
The manifestations of a spinal epidural abscess are often insidious, presenting a complex puzzle for both patients and healthcare providers. Early symptoms may include localized pain, tenderness, and stiffness in the affected area, mimicking more common spinal conditions. As the abscess progresses, systemic signs such as fever, chills, and malaise may emerge. Neurological symptoms, such as weakness, numbness, or tingling sensations, herald the potential impact on the spinal cord and nerve structures.
Diagnostic Challenges
Diagnosing a spinal epidural abscess poses a unique challenge due to the subtlety of its symptoms and the necessity for prompt intervention. Clinical suspicion, bolstered by imaging studies such as MRI or CT scans, becomes the linchpin of diagnosis. Blood cultures and laboratory analyses further aid in identifying the causative pathogens, paving the way for targeted treatment.
Treatment Strategies
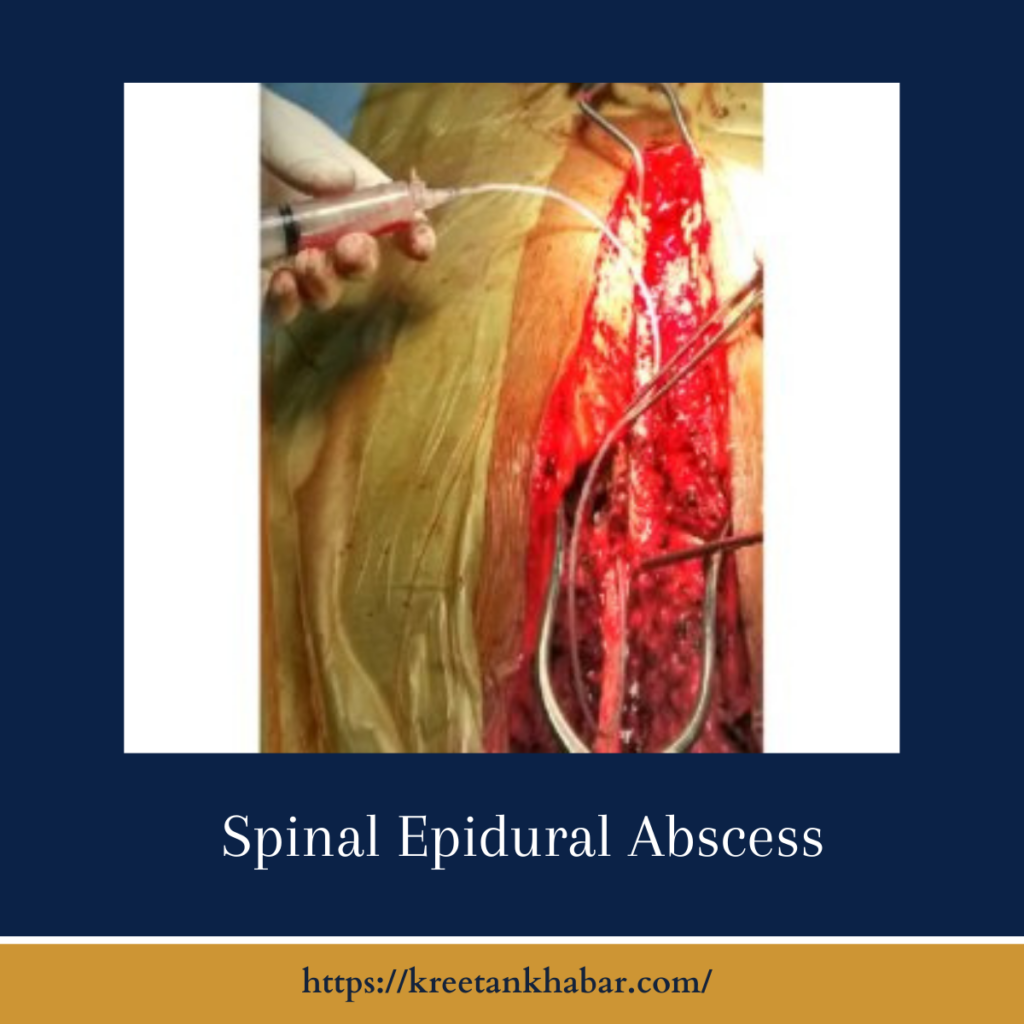
The treatment of a spinal epidural abscess is a delicate balancing act between addressing the infection and preventing neurological complications. Antibiotic or antifungal therapy, guided by the specific pathogen, forms the backbone of treatment. Surgical intervention may be warranted in cases of severe compression, abscess drainage, or when neurological deficits persist. The collaborative efforts of infectious disease specialists, neurosurgeons, and other healthcare professionals are crucial in sculpting an effective treatment plan.
Preventive Measures and Proactive Care
As the old adage goes, prevention is often the best cure. In the context of spinal epidural abscess, maintaining a vigilant stance involves addressing risk factors such as diabetes, immunosuppression, or intravenous drug use. Prompt attention to any signs of spinal infection or unusual neurological symptoms becomes paramount for early detection and intervention.
Conclusion
In the quiet recesses of the spinal canal, the enigma of a spinal epidural abscess unfolds, requiring a keen eye and swift action. As we navigate through the shadows of this stealthy intruder, the collaborative efforts of patients and healthcare providers become the beacon of hope. By unraveling the mysteries of its origins, recognizing the subtleties of its symptoms, and embracing timely interventions, we embark on a journey towards not just treatment but the restoration of spinal health and resilience. In this ongoing exploration, the tale of the spinal epidural abscess continues to be written, with each chapter contributing to a deeper understanding and more effective management of this intricate medical enigma.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023