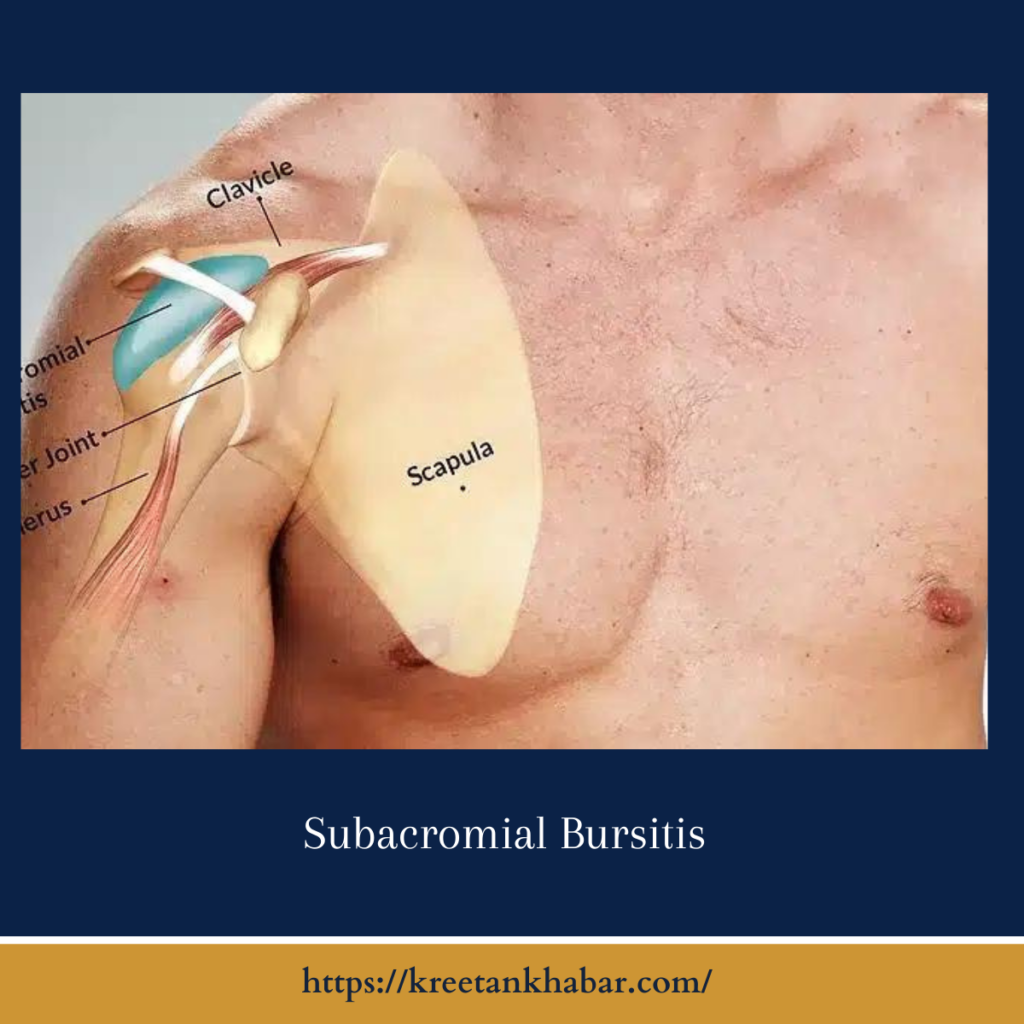
Subacromial Bursitis
Subacromial bursitis is a common yet often overlooked cause of shoulder pain and discomfort. Situated beneath the acromion, a bony prominence of the shoulder blade, the subacromial bursa serves as a lubricating cushion between the rotator cuff tendons and the overlying bone. When inflamed, typically due to repetitive overhead activities, trauma, or underlying conditions, the subacromial bursa can become swollen and painful, leading to restricted movement and functional impairment. In this article, we’ll delve into the intricacies of subacromial bursitis, exploring its causes, symptoms, diagnosis, and treatment options to provide clarity and guidance for individuals grappling with shoulder pain.
Understanding Subacromial Bursitis:
Subacromial bursitis is characterized by inflammation of the subacromial bursa, a fluid-filled sac that facilitates smooth movement of the rotator cuff tendons beneath the acromion. The primary role of the bursa is to reduce friction and provide cushioning during shoulder movement. However, when subjected to repetitive stress, trauma, or inflammatory conditions, such as arthritis or tendonitis, the bursa can become irritated and swollen, leading to pain and functional limitations.
Causes and Risk Factors:
Several factors can contribute to the development of subacromial bursitis, including:
- Repetitive Overhead Activities: Engaging in repetitive overhead movements, such as lifting weights, throwing, or reaching overhead, can strain the rotator cuff tendons and irritate the subacromial bursa, predisposing individuals to bursitis.
- Trauma or Injury: Direct trauma to the shoulder, such as a fall onto an outstretched arm or a sudden impact, can injure the subacromial bursa and trigger inflammation and swelling.
- Anatomical Factors: Structural abnormalities of the shoulder, such as bone spurs, acromial shape variations, or impingement of the rotator cuff tendons, can increase the risk of subacromial bursitis by narrowing the subacromial space and compressing the bursa.
- Poor Posture: Maintaining poor posture, such as rounded shoulders or forward head posture, can alter the biomechanics of the shoulder joint and contribute to shoulder impingement, leading to bursitis over time.
- Muscle Imbalance: Weakness or imbalance of the muscles surrounding the shoulder joint, including the rotator cuff muscles and scapular stabilizers, can disrupt normal shoulder mechanics and predispose individuals to bursitis.
- Age and Degenerative Changes: As individuals age, degenerative changes in the shoulder joint, such as osteoarthritis or degenerative tendon changes, can increase the risk of subacromial bursitis due to decreased joint mobility and tissue integrity.
Symptoms of Subacromial Bursitis:
The symptoms of subacromial bursitis can vary in severity and may include:
- Shoulder Pain: Persistent, localized pain in the shoulder, particularly with overhead movements or activities that compress the subacromial space, such as reaching or lifting.
- Shoulder Stiffness: Stiffness and limited range of motion in the shoulder joint, especially with activities that require elevation or external rotation of the arm.
- Swelling and Tenderness: Swelling, redness, and tenderness over the front and side of the shoulder, near the acromion, where the subacromial bursa is located.
- Pain at Rest: Discomfort and achiness in the shoulder, even at rest, particularly when lying on the affected side or applying pressure to the shoulder.
- Weakness and Instability: Weakness and instability in the shoulder, especially with activities that require lifting or carrying objects overhead, due to pain and functional limitations.
Diagnosis and Treatment:
Diagnosing subacromial bursitis typically involves a combination of clinical evaluation, medical history review, physical examination, and imaging studies such as X-rays, ultrasound, or MRI scans to assess the extent of inflammation and rule out other potential causes of shoulder pain. Treatment options for subacromial bursitis may include:
- Rest and Activity Modification: Resting the affected shoulder and avoiding activities that exacerbate pain or irritation, such as overhead lifting or repetitive reaching, can help alleviate symptoms and promote healing.
- Ice Therapy: Applying ice packs or cold therapy to the shoulder several times a day can help reduce pain, inflammation, and swelling associated with subacromial bursitis.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs such as ibuprofen or naproxen may be recommended to reduce pain and inflammation in the shoulder joint.
- Physical Therapy: A tailored physical therapy program focusing on stretching, strengthening, and proprioceptive exercises can improve shoulder mobility, stability, and function while addressing underlying biomechanical issues contributing to bursitis.
- Steroid Injections: Corticosteroid injections into the subacromial space may be administered to reduce inflammation and provide temporary pain relief for individuals with persistent symptoms despite conservative treatment measures.
- Ultrasound-Guided Aspiration: In cases of severe swelling or fluid accumulation within the subacromial bursa, ultrasound-guided aspiration may be performed to remove excess fluid and alleviate pressure on the surrounding tissues.
- Surgical Intervention: In refractory cases of subacromial bursitis that do not respond to conservative treatments, surgical intervention such as subacromial decompression or bursectomy may be considered to alleviate impingement and remove inflamed bursal tissue.
Rehabilitation and Recovery:
Rehabilitation and recovery from subacromial bursitis focus on restoring pain-free shoulder function, improving range of motion, and preventing recurrence of symptoms. Rehabilitation strategies may include:
- Range of Motion Exercises: Gradual progression of shoulder range of motion exercises, including passive and active-assisted movements, to restore flexibility and mobility in the shoulder joint.
- Strengthening Exercises: Progressive strengthening exercises targeting the rotator cuff muscles, scapular stabilizers, and shoulder girdle muscles to improve shoulder stability, muscle balance, and functional strength.
- Postural Correction: Emphasis on postural correction exercises and ergonomic modifications to address underlying muscle imbalances and promote proper alignment of the shoulder joint during daily activities.
- Functional Training: Integration of functional training exercises and activities of daily living to simulate real-life movements and enhance shoulder function, coordination, and proprioception.
- Activity Modification: Education on proper body mechanics, lifting techniques, and activity modification strategies to prevent re-injury and minimize strain on the shoulder joint during work, sports, and recreational activities.
- Patient Education: Comprehensive education on the underlying causes of subacromial bursitis, self-management strategies, and long-term preventive measures to empower individuals in managing their condition and reducing the risk of recurrence.
Preventive Measures:
Preventing subacromial bursitis requires a proactive approach that addresses modifiable risk factors, promotes shoulder health, and emphasizes injury prevention strategies. Key preventive measures include:
- Proper Warm-Up: Prior to engaging in physical activity, perform a thorough warm-up routine consisting of dynamic stretching, mobility exercises, and shoulder-specific warm-up drills to prepare the muscles and joints for activity.
- Progressive Loading: Gradually increase the intensity, duration, and frequency of physical activities and exercises to allow the shoulder muscles and tissues to adapt and strengthen over time, reducing the risk of overuse injuries such as bursitis.
- Technique Correction: Ensure proper technique and form during sports, weightlifting, and occupational tasks to minimize excessive stress and strain on the shoulder joint and surrounding structures.
- Cross-Training: Incorporate cross-training activities and exercises that target different muscle groups and movement patterns to promote overall musculoskeletal health, prevent muscular imbalances, and reduce the risk of overuse injuries.
- Ergonomic Modifications: Make ergonomic adjustments to workstations, equipment, and tools to promote proper posture, reduce repetitive strain, and alleviate shoulder stress during prolonged periods of sitting, typing, or performing manual tasks.
- Regular Exercise: Maintain a regular exercise routine that includes shoulder-strengthening exercises, flexibility exercises, and cardiovascular activities to improve overall fitness, enhance shoulder stability, and reduce the risk of musculoskeletal injuries.
Conclusion:
In conclusion, subacromial bursitis is a common source of shoulder pain and dysfunction that can significantly impact daily activities and quality of life. By understanding the underlying causes, symptoms, diagnosis, and treatment options for subacromial bursitis, individuals can take proactive steps to manage their condition effectively and prevent recurrence. Through a comprehensive approach that includes conservative treatments, rehabilitation strategies, and preventive measures, individuals with subacromial bursitis can achieve pain relief, restore shoulder function, and return to their desired level of activity with confidence and resilience.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023