Subdural Hematoma: A Closer Look at the Silent Intruder
Introduction:
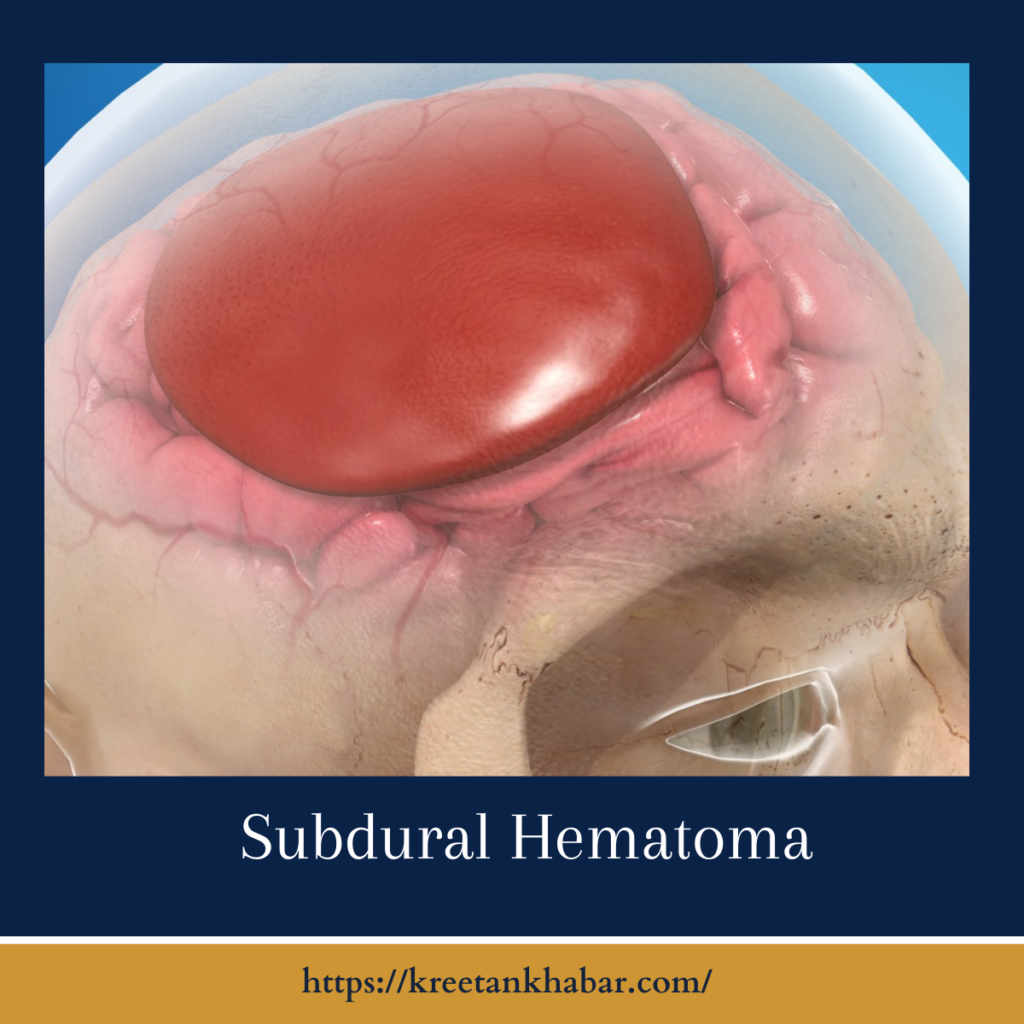
In the intricate landscape of neurological disorders, subdural hematoma emerges as a clandestine threat, silently infiltrating the delicate confines of the brain. This condition, marked by the accumulation of blood between the brain and its outermost covering, the dura mater, often conceals its presence until symptoms manifest. As we delve into the depths of subdural hematoma, we unravel the enigma surrounding this condition, exploring its causes, symptoms, and treatment options.
Understanding Subdural Hematoma:
Subdural hematoma is a medical condition characterized by the accumulation of blood in the space between the brain and the dura mater—the protective membrane covering the brain. This bleeding typically results from the rupture of tiny blood vessels bridging the brain and its outer covering. The blood gradually pools, exerting pressure on the brain and potentially leading to a range of symptoms.
Causes:
A myriad of factors can contribute to the development of subdural hematoma. Traumatic events, such as falls, car accidents, or blunt force injuries to the head, are common triggers. However, spontaneous subdural hematomas can also occur, especially in older adults, where blood vessels may be more fragile. Chronic conditions like hemophilia, anticoagulant medication use, and certain diseases affecting blood clotting may further elevate the risk.
Symptoms:
One of the challenges posed by subdural hematoma lies in its ability to remain asymptomatic initially. The gradual nature of blood accumulation allows the body to adapt to the increased pressure, delaying the onset of noticeable signs. When symptoms do emerge, they may include persistent headaches, confusion, difficulty concentrating, and, in severe cases, seizures or loss of consciousness.
- Gradual Onset of Headaches:
- Subdural hematoma often begins its subtle assault with persistent headaches. These headaches may start mildly and gradually intensify over time, serving as an early warning sign.
- Cognitive Impairment:
- As the hematoma exerts pressure on the brain, cognitive functions may become compromised. Individuals might experience difficulties with concentration, memory lapses, and an overall sense of mental fogginess.
- Altered Mental Status:
- Changes in mental status, ranging from confusion to significant alterations in consciousness, can signal the progression of subdural hematoma. This may manifest as disorientation, drowsiness, or an inability to stay alert.
- Personality Changes:
- Friends and family may notice subtle or pronounced alterations in personality. These changes can include irritability, mood swings, or a shift in behavior that is inconsistent with the individual’s typical demeanor.
- Nausea and Vomiting:
- Increased intracranial pressure resulting from the hematoma can cause nausea and vomiting. These symptoms may be persistent and unrelated to other digestive issues.
- Seizures:
- In more severe cases, subdural hematoma can trigger seizures. These episodes may be a consequence of the pressure on the brain affecting normal electrical activity.
- Weakness or Numbness:
- As the hematoma progresses, it may impinge on specific areas of the brain responsible for motor function. This can lead to weakness or numbness, often affecting one side of the body more than the other.
- Difficulty Walking:
- The coordination centers in the brain may be compromised, resulting in difficulty walking or maintaining balance. This symptom can contribute to an increased risk of falls.
- Visual Disturbances:
- Pressure on the optic nerve or other visual processing areas can cause changes in vision. Blurred vision, double vision, or difficulty focusing on objects may be indicative of a developing subdural hematoma.
- Sudden Loss of Consciousness:
- In severe cases, the hematoma can rapidly escalate, leading to a sudden loss of consciousness. This is a medical emergency requiring immediate attention.
- Delayed Symptom Presentation:
- One of the challenges with subdural hematoma is its ability to remain asymptomatic initially. Symptoms may not become apparent until days or weeks after the initial injury, making early detection and diagnosis crucial.
- Worsening Symptoms Over Time:
- The symptoms of subdural hematoma often progress gradually, worsening over time as the blood accumulation increases. Monitoring for any changes in neurological function is essential for timely intervention.
Recognizing the diverse array of symptoms associated with subdural hematoma is vital for early diagnosis and intervention. Whether it’s the insidious onset of headaches or more pronounced neurological deficits, paying attention to these signs can make a significant difference in the outcome for individuals affected by this condition.
Diagnosis:
Given its subtle presentation, diagnosing subdural hematoma requires a comprehensive approach. Neurological examinations, imaging studies such as CT scans or MRIs, and a detailed patient history are crucial components of the diagnostic process. Understanding the circumstances leading to head injury or identifying underlying health conditions becomes paramount in unveiling the mystery of this silent intruder.
Treatment Options:
The management of subdural hematoma hinges on the severity of symptoms, the size of the hematoma, and the overall health of the patient. Mild cases may resolve spontaneously or with conservative measures, while more severe instances may necessitate surgical intervention. Drainage procedures, such as burr hole surgery or craniotomy, aim to alleviate pressure on the brain and evacuate accumulated blood.
Prognosis and Rehabilitation:
The prognosis for individuals with subdural hematoma varies, depending on factors such as age, overall health, and the promptness of intervention. While some may experience a full recovery, others may contend with lingering neurological deficits. Rehabilitation often plays a crucial role in restoring cognitive function, motor skills, and overall quality of life for those affected.
Conclusion:
Subdural hematoma, with its stealthy onset and potentially devastating consequences, underscores the delicate nature of the human brain. Awareness of risk factors, prompt diagnosis, and appropriate treatment are pivotal in unraveling the enigma of this silent intruder. As we continue to delve into the complexities of neurological health, our understanding of subdural hematoma grows, paving the way for enhanced prevention, diagnosis, and treatment strategies.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023