Ulcerative Colitis: Understanding Symptoms, Causes, and Management
Introduction:
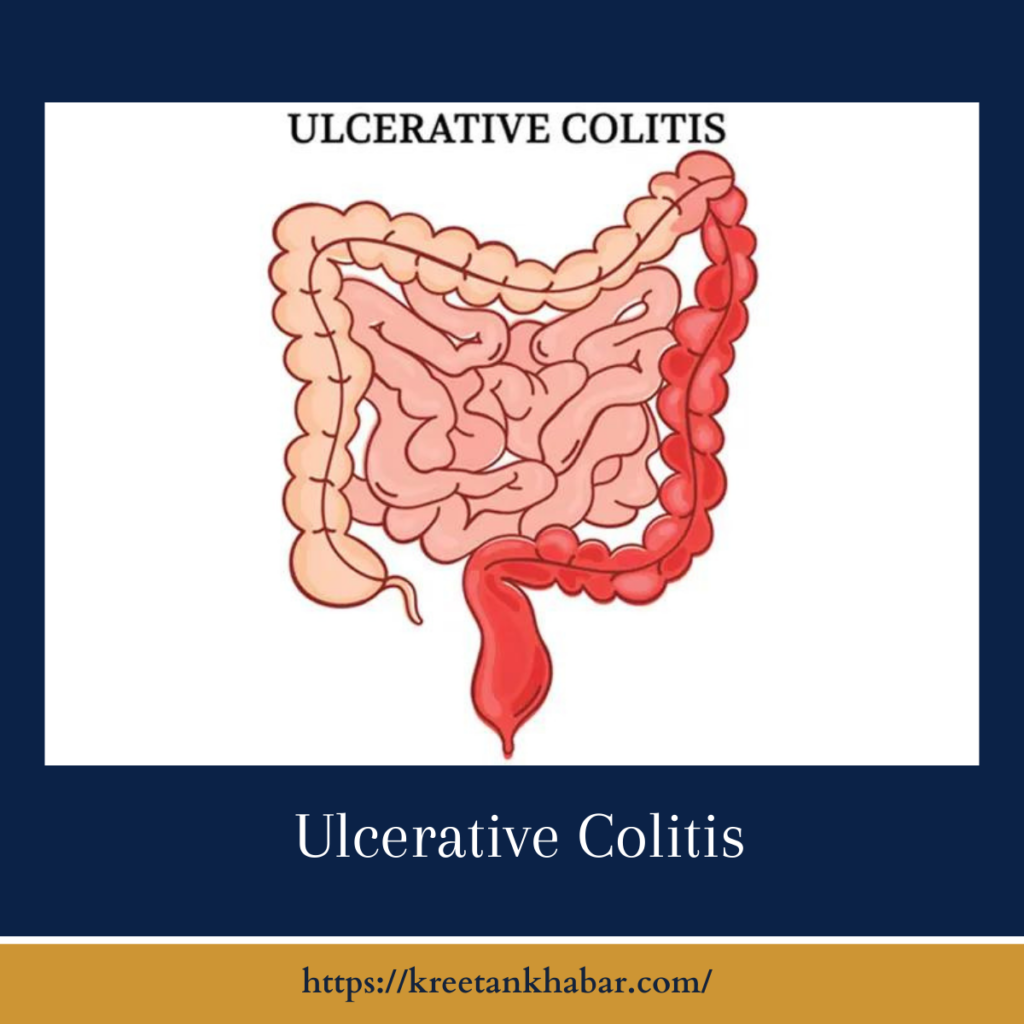
Ulcerative (UC) is a chronic inflammatory bowel disease (IBD) that affects the colon and rectum, leading to a range of symptoms and challenges for those diagnosed. While the exact cause of Ulcerative remains elusive, advancements in medical understanding and treatment options offer hope for effective management. In this article, we explore the intricacies of Ulcerative Colitis, shedding light on its symptoms, potential causes, and strategies for coping with this complex condition.
Understanding Ulcerative Colitis:
Ulcerative Colitis is characterized by inflammation and ulcers in the lining of the colon and rectum. This chronic condition is one of the two main forms of inflammatory bowel disease, the other being Crohn’s disease. While Crohn’s can affect any part of the digestive tract, Ulcerative specifically targets the colon and rectum.
Symptoms of Ulcerative Colitis:
- Diarrhea: Persistent and often bloody diarrhea is a common symptom of Ulcerative. The inflammation in the colon results in an increased urgency to have bowel movements.
- Abdominal Pain: Cramping and abdominal pain, particularly in the lower left side, are frequent symptoms. The severity of pain can vary and may be relieved temporarily after a bowel movement.
- Rectal Bleeding: Blood in the stool is a hallmark symptom of Ulcerative. The inflammation and ulceration in the colon’s lining lead to bleeding during bowel movements.
- Weight Loss: Chronic inflammation and diarrhea can contribute to weight loss and malnutrition over time.
- Fatigue: Persistent inflammation and the body’s response to the condition can lead to fatigue, even with sufficient rest.
- Loss of Appetite: The symptoms of Ulcerative, including abdominal pain and discomfort, can contribute to a loss of appetite.
- Fever: Some individuals with Ulcerative may experience fever, particularly during periods of active inflammation.
- Joint Pain: Joint pain and inflammation, known as arthralgia, can occur in some individuals with Ulcerative.
Potential Causes of Ulcerative Colitis:
- Immune System Dysfunction: Ulcerative is believed to result from an abnormal immune response, where the immune system mistakenly attacks the healthy cells of the digestive tract, leading to inflammation.
- Genetic Factors: There is evidence to suggest a genetic predisposition to Ulcerative. Individuals with a family history of IBD may be at a higher risk.
- Environmental Factors: Environmental factors, such as exposure to certain bacteria or viruses, may play a role in triggering Ulcerative, especially in individuals with a genetic susceptibility.
- Dysregulation of Gut Microbiota: Imbalances in the gut microbiota, the trillions of microbes residing in the digestive tract, have been implicated in the development of Ulcerative.
The more points of Potential causes:
- Immune System Dysfunction: Ulcerative Colitis (UC) is believed to stem from an abnormal immune response where the immune system mistakenly attacks the healthy cells of the digestive tract. This results in chronic inflammation and ulceration in the colon and rectum.
- Genetic Predisposition: There is evidence to suggest a genetic component to Ulcerative. Individuals with a family history of inflammatory bowel disease (IBD), including Ulcerative, may have a higher risk of developing the condition. Certain genetic variations are associated with an increased susceptibility to Ulcerative.
- Environmental Factors: Environmental factors may contribute to the development of Ulcerative, especially in individuals with a genetic predisposition. Exposure to specific bacteria or viruses, as well as environmental triggers, could play a role in initiating or exacerbating the inflammatory response in the digestive tract.
- Dysregulation of Gut Microbiota: Imbalances in the gut microbiota, the complex community of microorganisms residing in the digestive tract, have been implicated in the pathogenesis of Ulcerative Colitis. Disruptions in the balance of beneficial and harmful bacteria may contribute to an exaggerated immune response and chronic inflammation.
- Autoimmune Response: Ulcerative is considered an autoimmune disease, wherein the body’s immune system mistakenly targets and attacks its own tissues. In the case of Ulcerative Colitis, the immune system targets the lining of the colon and rectum, leading to inflammation and the characteristic symptoms of the condition.
- Epigenetic Factors: Epigenetic changes, alterations in gene expression that do not involve changes to the underlying DNA sequence, may play a role in Ulcerative. Environmental factors, lifestyle, and diet can influence epigenetic modifications, potentially impacting the development and course of the disease.
- Smoking: Smoking has been identified as a unique factor in Ulcerative, with some studies suggesting that it may have a protective effect against the development of Ulcerative Colitis. However, the relationship between smoking and UC is complex, and quitting smoking is generally advised for overall health.
- Medication-Induced: In some cases, certain medications may trigger the onset of Ulcerative or exacerbate existing symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) are examples of medications that may contribute to inflammation in the digestive tract.
- Stress and Psychological Factors: While stress does not directly cause Ulcerative, it can influence disease activity and exacerbate symptoms. Psychological factors, such as chronic stress or a history of traumatic events, may impact the course of UC in susceptible individuals.
- Dietary Factors: While diet alone does not cause Ulcerative, certain dietary factors may influence disease activity. Individuals with Ulcerative Colitis may find that certain foods, such as spicy foods or dairy products, can trigger or worsen symptoms.
Understanding the multifactorial nature of Ulcerative, including the interplay between genetic, environmental, and immunological factors, is crucial for developing effective treatment strategies and interventions. Ongoing research continues to deepen our understanding of the complex mechanisms underlying the development and progression of Ulcerative Colitis.
Management of Ulcerative Colitis:
- Medications: Various medications, including anti-inflammatory drugs, immunosuppressants, and biologics, may be prescribed to manage symptoms and control inflammation.
- Lifestyle Modifications: Dietary changes, such as avoiding trigger foods, maintaining a well-balanced diet, and staying hydrated, can help manage symptoms.
- Supplements: Some individuals with Ulcerative may benefit from nutritional supplements, such as iron, calcium, and vitamin D, to address deficiencies.
- Stress Management: Stress can exacerbate Ulcerative symptoms, so stress management techniques, such as meditation, yoga, or counseling, may be beneficial.
- Surgery: In severe cases or when medications are ineffective, surgery to remove the colon (colectomy) may be recommended.
- Regular Monitoring: Ongoing monitoring through regular check-ups and diagnostic tests helps assess disease activity and adjust treatment plans accordingly.
- Support Groups: Joining support groups or seeking counseling can provide emotional support and practical insights for individuals living with Ulcerative.
Conclusion:
Ulcerative Colitis is a chronic condition that requires a comprehensive and personalized approach to management. By understanding the symptoms, potential causes, and available treatment options, individuals with Ulcerative can work collaboratively with healthcare professionals to navigate the challenges of the condition. Ongoing research and advancements in medical science continue to enhance our understanding of Ulcerative, offering hope for improved outcomes and an enhanced quality of life for those affected by this complex inflammatory bowel disease.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023