Understanding Ovarian Cysts: Causes, Symptoms, and Treatment
Introduction
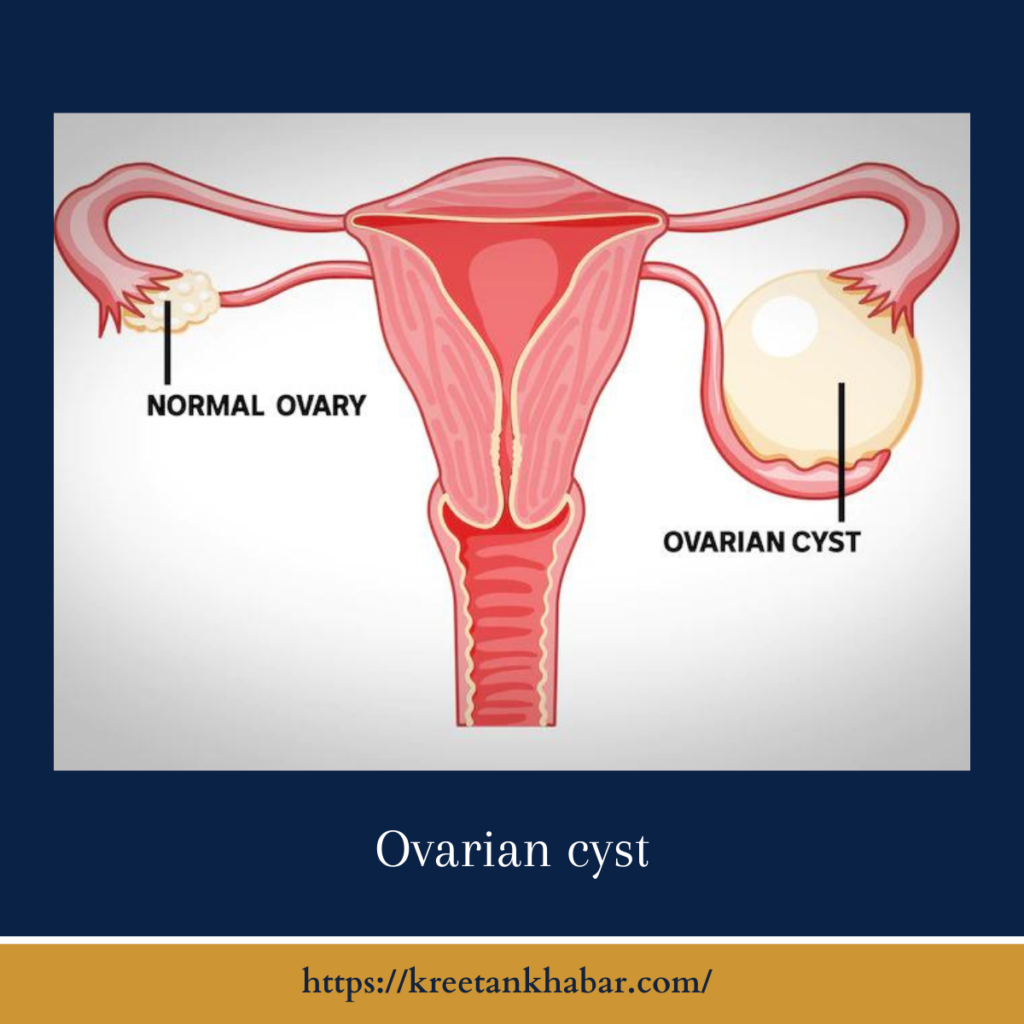
Ovarian cysts are common fluid-filled sacs that can form in or on the ovaries of women. While most ovarian cysts are harmless and resolve on their own, some may cause discomfort or health complications. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for ovarian cysts.
What Are Ovarian Cysts?
Ovarian cysts are small, fluid-filled sacs that develop within or on the ovaries, which are part of the female reproductive system. These cysts can vary in size, ranging from as small as a pea to several centimeters in diameter. While many ovarian cysts are benign (non-cancerous), some may cause symptoms or complications.
Causes of Ovarian Cysts
Ovarian cysts can develop for various reasons, including:
- Functional Cysts: The most common type of ovarian cysts, these form as part of the menstrual cycle. They include:
- Follicular Cysts: When an ovarian follicle fails to release an egg during ovulation and continues to grow.
- Corpus Luteum Cysts: After ovulation, the follicle may become a corpus luteum cyst. These typically resolve on their own but can occasionally bleed or twist, causing pain.
- Dermoid Cysts: These cysts contain tissues such as hair, skin, and teeth and can develop from embryonic cells.
- Cystadenomas: These cysts form from the cells on the outer surface of the ovaries and can grow quite large.
- Endometriomas: When endometrial tissue (the tissue lining the uterus) grows on the ovaries, it can form cysts known as endometriomas.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS often have multiple small cysts on their ovaries due to hormonal imbalances.
here are key points outlining the potential causes of ovarian cysts:
- Functional Cysts:
- Follicular Cysts: These cysts form during the normal menstrual cycle when an ovarian follicle fails to release an egg during ovulation and continues to grow.
- Corpus Luteum Cysts: After ovulation, the follicle transforms into a corpus luteum cyst, which typically resolves on its own but can occasionally cause pain or complications.
- Dermoid Cysts:
- These cysts, also known as mature teratomas, contain various types of tissues, including hair, skin, and teeth.
- They develop from embryonic cells and are typically benign.
- Cystadenomas:
- Cystadenomas are cysts that originate from the cells on the outer surface of the ovaries.
- They can become quite large and may be filled with mucous or other fluids.
- Endometriomas:
- When endometrial tissue (the tissue lining the uterus) grows abnormally on the ovaries, it can form cysts called endometriomas.
- These cysts are often associated with endometriosis.
- Polycystic Ovary Syndrome (PCOS):
- PCOS is a hormonal disorder characterized by the presence of multiple small cysts on the ovaries.
- It results from imbalances in hormones, including elevated levels of androgens (male hormones).
- Iatrogenic Cysts:
- Some ovarian cysts may develop as a side effect of fertility treatments or hormone therapies.
- Tumors:
- Rarely, ovarian cysts may be associated with ovarian tumors, which can be benign or malignant.
- Infection:
- Infections in the pelvic area can sometimes lead to the formation of cysts.
- Torsion:
- Ovarian torsion occurs when a cyst causes the ovary to twist, potentially cutting off its blood supply and causing pain.
- Hormonal Imbalances:
- Fluctuations in hormone levels, such as those that occur during the menstrual cycle, can contribute to the development of cysts.
It’s important to note that while these are some common causes of ovarian cysts, many cysts resolve on their own without causing symptoms or complications. The management and treatment of ovarian cysts depend on their type, size, and whether they are causing symptoms or other health issues.
Common Symptoms
Many ovarian cysts do not cause noticeable symptoms and are discovered incidentally during routine pelvic exams or imaging tests. However, when symptoms do occur, they may include:
- Pelvic Pain: Dull, aching, or sharp pain in the lower abdomen or pelvis, which may be constant or intermittent.
- Bloating or Fullness: A feeling of abdominal bloating or fullness.
- Changes in Menstrual Periods: Irregular periods, heavier or lighter bleeding, or spotting between periods.
- Pain During Intercourse: Discomfort or pain during sexual intercourse.
- Frequent Urination: Increased urge to urinate, often due to cyst pressure on the bladder.
- Difficulty Emptying the Bladder or Bowels: Large cysts can exert pressure on nearby organs, causing discomfort.
Diagnosis
The diagnosis of ovarian cysts typically involves:
- Pelvic Examination: A healthcare provider may detect ovarian cysts during a routine pelvic exam.
- Ultrasound: Transvaginal or abdominal ultrasound can provide detailed images of the ovaries, helping determine the size, location, and type of cyst.
- Blood Tests: CA-125 blood test may be done to assess ovarian cancer risk in postmenopausal women with complex cysts.
- MRI or CT Scan: In some cases, additional imaging tests may be ordered to gain more information about the cysts.
Treatment Options
The treatment of ovarian cysts depends on several factors, including the type of cyst, its size, and whether it is causing symptoms. Treatment options may include:
- Watchful Waiting: For small, asymptomatic cysts, healthcare providers may recommend regular monitoring to see if they resolve on their own.
- Pain Management: Over-the-counter pain relievers may be used to manage mild discomfort.
- Birth Control Pills: Hormonal birth control can help regulate the menstrual cycle and prevent the formation of new cysts.
- Surgical Removal: Large cysts, cysts that persist or grow, or those causing severe symptoms may require surgical removal (cystectomy or oophorectomy).
- Laparoscopy: Minimally invasive surgery may be used to remove cysts while preserving the ovaries.
- Treatment for PCOS: PCOS-related cysts may be managed with lifestyle changes, hormone therapy, or medications to improve insulin sensitivity.
here are key points outlining the treatment options for ovarian cysts:
- Watchful Waiting:
- Small, asymptomatic ovarian cysts often resolve on their own without medical intervention.
- Healthcare providers may recommend regular monitoring through ultrasound to track changes in the cyst’s size or characteristics.
- Pain Management:
- Over-the-counter pain relievers such as ibuprofen or acetaminophen may be used to alleviate mild discomfort associated with ovarian cysts.
- Hormonal Birth Control:
- Hormonal birth control methods, such as birth control pills, patches, or hormonal intrauterine devices (IUDs), may help regulate the menstrual cycle and prevent the formation of new cysts.
- Continuous birth control use may reduce the likelihood of functional cysts.
- Surgical Removal (Cystectomy):
- Large, persistent, or complex cysts, or those causing severe symptoms, may require surgical removal.
- Cystectomy is a procedure where only the cyst is removed while preserving the affected ovary.
- Oophorectomy:
- In some cases, when the cyst is associated with a tumor, or if there are concerns about malignancy, the entire ovary may be removed through surgery, known as an oophorectomy.
- Laparoscopy:
- Laparoscopic surgery is a minimally invasive approach to remove ovarian cysts.
- Small incisions are made, and a thin, lighted instrument is used to remove the cyst while preserving the ovary.
- Aspiration (Drainage):
- In cases of large cysts or cysts causing acute pain, fluid may be drained from the cyst through a needle inserted into the abdomen.
- This procedure is known as cyst aspiration or cyst drainage.
- Hormone Therapy:
- Hormone therapy using gonadotropin-releasing hormone (GnRH) agonists may be considered to shrink cysts associated with endometriosis.
- This treatment is typically used when other options are ineffective or to provide temporary relief.
- Treatment for Polycystic Ovary Syndrome (PCOS):
- Management of PCOS-related cysts involves addressing the underlying hormonal imbalances.
- Lifestyle modifications, such as weight management, dietary changes, and exercise, may be recommended.
- Hormonal medications, like birth control pills or anti-androgen drugs, can help regulate menstrual cycles and reduce cyst formation.
- Follow-Up and Monitoring:
- Regardless of the treatment approach, regular follow-up appointments and monitoring are essential to assess the effectiveness of treatment, check for recurrence, and ensure the overall health of the ovaries.
The choice of treatment depends on various factors, including the type and size of the cyst, its impact on a person’s health and quality of life, and individual preferences. It is important for individuals with ovarian cysts to discuss their options with a healthcare provider to determine the most suitable treatment plan.
Conclusion
Ovarian cysts are a common occurrence in women, and most of them are benign and harmless. However, when symptoms arise or cysts become large or complex, medical evaluation and treatment may be necessary. Regular check-ups and communication with a healthcare provider are essential to monitor any changes in ovarian health and address any concerns promptly.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023