Understanding Pelvic Organ Prolapse: Causes, Symptoms, and Treatment Options
Introduction
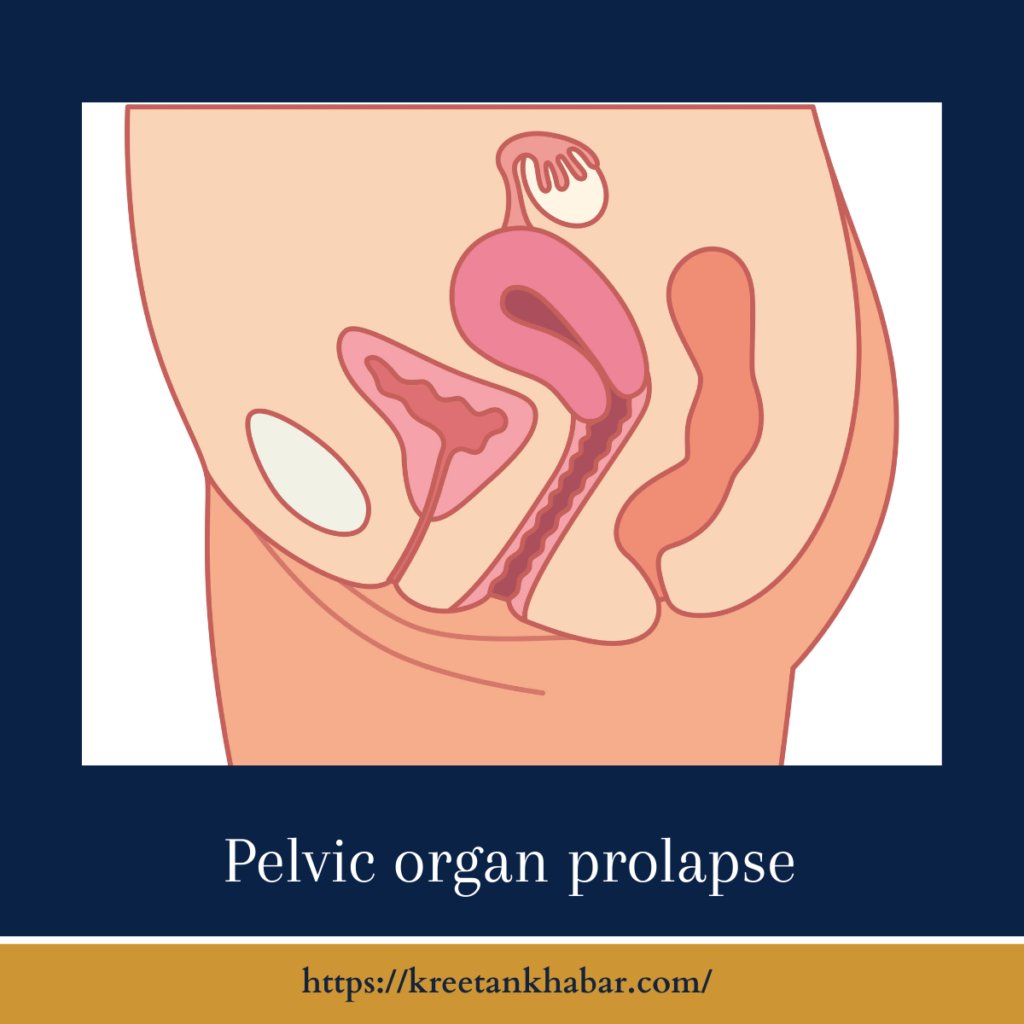
Pelvic organ prolapse (POP) is a common medical condition that primarily affects women, especially as they age or after childbirth. It occurs when one or more pelvic organs, such as the uterus, bladder, or rectum, descend or bulge into the vaginal wall due to weakened pelvic floor muscles and ligaments. While POP can be uncomfortable and distressing, there are various treatment options available to manage and alleviate its symptoms. In this article, we will explore the causes, symptoms, and treatment options for pelvic organ prolapse.
The Causes of Pelvic Organ Prolapse
- Childbirth: One of the most significant risk factors for POP is childbirth, especially multiple vaginal deliveries. The stretching and weakening of pelvic floor muscles during labor and delivery can contribute to prolapse later in life.
- Aging: As women age, hormonal changes, collagen loss, and the natural weakening of pelvic tissues can increase the risk of POP.
- Menopause: Reduced estrogen levels during menopause can further weaken the pelvic muscles and support structures, potentially leading to prolapse.
- Chronic Straining: Chronic conditions that require frequent straining during bowel movements (e.g., constipation) or chronic coughing can weaken the pelvic floor muscles over time.
- Obesity: Excess body weight can place additional pressure on the pelvic organs and weaken the supporting structures.
- Genetic Factors: Some individuals may have a genetic predisposition to weaker pelvic tissues, making them more susceptible to POP.
- Hysterectomy: Surgical removal of the uterus (hysterectomy) can alter pelvic support, increasing the risk of prolapse in some cases.
Common Symptoms of Pelvic Organ Prolapse
The symptoms of pelvic organ prolapse can vary in severity and may include:
- Vaginal Bulging: A noticeable bulge or lump in the vaginal area is a common symptom, which may vary in size and position depending on the affected organ(s).
- Pelvic Pressure: A feeling of fullness or pressure in the pelvic region, akin to a heaviness or dragging sensation.
- Urinary Symptoms: POP can lead to urinary problems, including frequent urination, urgency, incontinence, or difficulty emptying the bladder.
- Bowel Symptoms: Constipation, straining during bowel movements, or fecal incontinence may occur when the rectum is affected by prolapse.
- Pain or Discomfort: Some individuals may experience discomfort, pain, or an ache in the lower abdomen, lower back, or pelvis.
- Painful Intercourse: Sexual discomfort or pain during intercourse is common with certain types of POP.
- Vaginal Bleeding or Spotting: In cases of uterine prolapse, some women may experience vaginal bleeding or spotting.
Treatment Options for Pelvic Organ Prolapse
- Pelvic Floor Exercises (Kegels): Regularly performing pelvic floor exercises, known as Kegel exercises, can help strengthen the pelvic muscles and provide symptom relief.
- Physical Therapy: Pelvic floor physical therapy, under the guidance of a specialized therapist, can teach techniques to strengthen and support pelvic muscles.
- Pessaries: A pessary is a device inserted into the vagina to provide support to the pelvic organs and alleviate symptoms.
- Hormone Replacement Therapy (HRT): In postmenopausal women, hormone replacement therapy may help improve the strength and flexibility of pelvic tissues.
- Lifestyle Modifications: Maintaining a healthy weight, managing chronic constipation, and avoiding heavy lifting can reduce the risk of POP worsening.
- Surgical Intervention: In cases of severe prolapse or when conservative treatments are ineffective, surgery may be necessary to repair and restore the pelvic organs to their proper position.
Here are 20 unique points describing treatment options for pelvic organ prolapse:
- Pelvic Floor Exercises (Kegels): Regularly practicing Kegel exercises can strengthen the pelvic floor muscles and improve support for the pelvic organs.
- Physical Therapy: Pelvic floor physical therapy, often guided by a specialized therapist, includes targeted exercises and techniques to enhance pelvic muscle strength and function.
- Pessary Use: A pessary is a device that can be inserted into the vagina to provide support for the displaced pelvic organs and alleviate symptoms of prolapse.
- Hormone Replacement Therapy (HRT): Hormone replacement therapy, particularly estrogen therapy, may be considered in postmenopausal women to improve pelvic tissue elasticity and resilience.
- Lifestyle Modifications: Adopting a healthy lifestyle that includes maintaining a healthy weight, managing chronic constipation, and avoiding heavy lifting can help prevent worsening of pelvic organ prolapse.
- Dietary Fiber: Incorporating a high-fiber diet can help alleviate constipation, which can contribute to prolapse symptoms.
- Biofeedback: Biofeedback therapy can help patients learn to control and strengthen their pelvic floor muscles by providing real-time feedback.
- Topical Estrogen Cream: For postmenopausal women, topical estrogen cream applied to the vaginal area can improve tissue health and reduce symptoms.
- Vaginal Inserts: In some cases, vaginal inserts or support devices can be used to help lift and support the prolapsed organs.
- Minimally Invasive Procedures: Minimally invasive surgical procedures, such as laparoscopic sacrocolpopexy or robotic-assisted surgery, can provide more extensive support and repair while minimizing recovery time.
- Hysterectomy: In cases where the uterus is a significant contributor to the prolapse, surgical removal (hysterectomy) may be recommended.
- Sacrocolpopexy: A surgical procedure that uses mesh or tissue grafts to support and reposition the prolapsed pelvic organs.
- Colporrhaphy: This surgical procedure involves repairing and tightening the vaginal walls to provide additional support to the pelvic organs.
- Vaginal Obliterative Surgery: Vaginal obliteration, or closure, may be considered in women who no longer desire vaginal intercourse and wish to alleviate symptoms.
- Uterosacral Ligament Suspension: A surgical procedure that involves reattaching and tightening the ligaments that support the uterus, bladder, and rectum.
- Perineorrhaphy: Surgical repair of the perineum, the area between the vagina and the anus, to improve pelvic floor support.
- Urogynecological Consultation: Consulting a urogynecologist, a specialist in female pelvic medicine and reconstructive surgery, can provide tailored treatment recommendations.
- Combined Procedures: In complex cases, a combination of surgical procedures may be necessary to address multiple prolapsed organs.
- Postoperative Physical Therapy: After surgery, pelvic floor physical therapy can aid in recovery and help patients regain strength and function.
- Regular Follow-Up: Women with pelvic organ prolapse should have regular follow-up appointments with their healthcare providers to monitor their condition and adjust treatment as needed.
Treatment options for pelvic organ prolapse vary based on the severity of the condition, the patient’s overall health, and individual preferences. Consulting with a healthcare provider or urogynecologist is essential to determine the most suitable treatment plan.
Conclusion
Pelvic organ prolapse is a common condition that can significantly impact a woman’s quality of life. Understanding its causes, recognizing the symptoms, and exploring available treatment options are essential steps toward managing and alleviating the discomfort associated with POP. Women experiencing symptoms of pelvic organ prolapse should seek guidance from a healthcare provider to determine the most appropriate treatment plan for their individual needs.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023