Understanding Soft Tissue Sarcomas: Types, Symptoms, and Treatment
Introduction
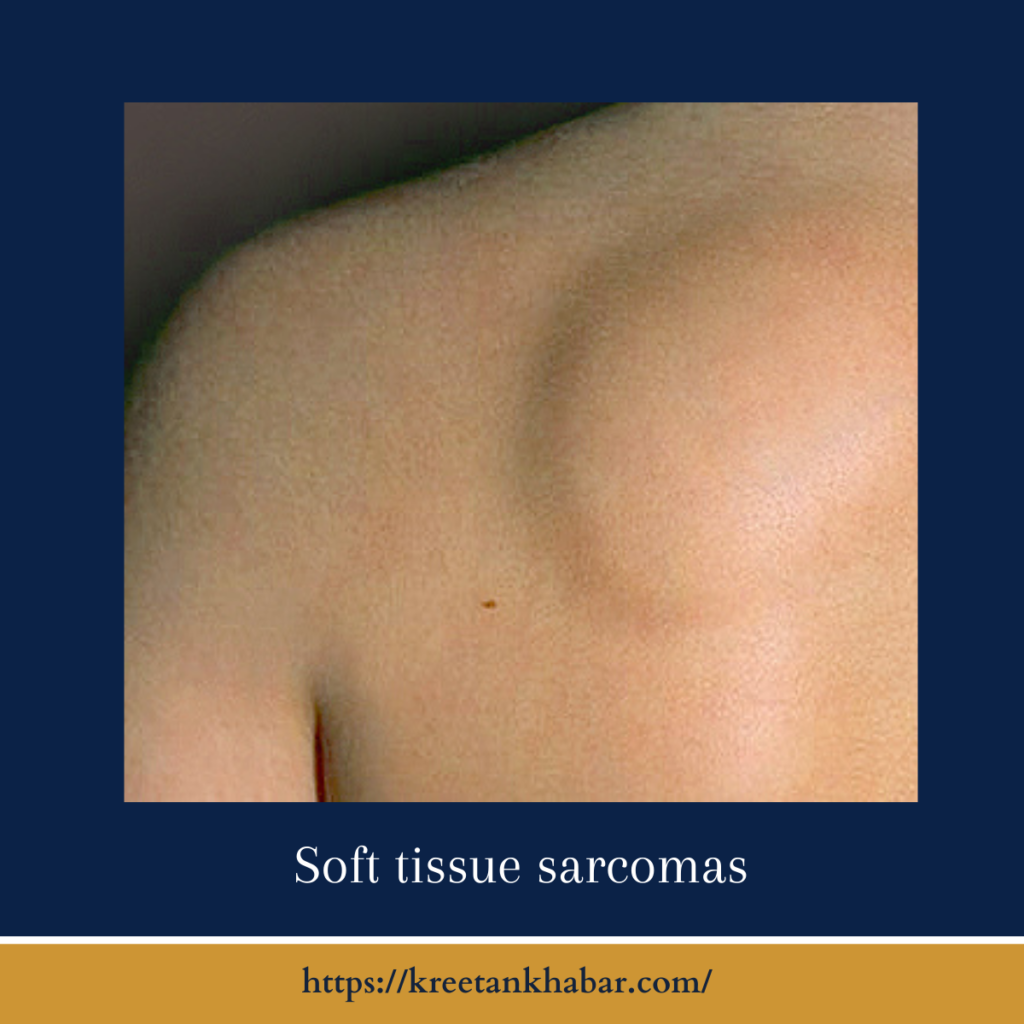
Soft tissue sarcomas are a diverse group of rare cancers that develop in the soft tissues of the body, including muscles, tendons, fat, and blood vessels. While relatively uncommon compared to more prevalent cancer types, understanding soft tissue sarcomas is essential for early diagnosis and effective treatment. In this article, we will explore the types, symptoms, risk factors, diagnosis, and treatment options for soft tissue sarcomas.
Types of Soft Tissue Sarcomas:
Soft tissue sarcomas encompass over 50 different subtypes, each originating from distinct types of soft tissue cells. Some common types include:
- Leiomyosarcoma: Arising from smooth muscle cells, often found in the uterus, gastrointestinal tract, or blood vessels.
- Liposarcoma: Developing from fat cells, typically found in the thighs, abdomen, or retroperitoneum (the space behind the abdomen).
- Rhabdomyosarcoma: Originating in skeletal muscle cells, this type is more common in children.
- Synovial Sarcoma: Occurring near joints in the arms or legs, it arises from cells in the synovial lining.
Symptoms of Soft Tissue Sarcomas:
- Lump or Mass: The most common sign is the discovery of a painless lump or mass in the affected area, often growing over time.
- Pain or Discomfort: As the tumor enlarges, it may press against nerves or surrounding structures, causing pain or discomfort.
- Limited Mobility: Depending on the tumor’s location, it may restrict the range of motion in nearby joints or muscles.
- Swelling or Edema: Swelling can occur, especially if the tumor affects lymphatic vessels.
- Unexplained Weight Loss: In advanced cases, unexplained weight loss and fatigue may occur.
Risk Factors:
While the exact cause of soft tissue sarcomas is often unknown, some factors may increase the risk:
- Radiation Exposure: Prior radiation therapy, especially in childhood, can raise the risk of soft tissue sarcomas.
- Genetic Syndromes: Certain genetic conditions, like Li-Fraumeni syndrome or neurofibromatosis, can predispose individuals to soft tissue sarcomas.
- Chemical Exposure: Rarely, exposure to specific chemicals and toxins may be linked to soft tissue sarcoma development.
here are key points about the risk factors associated with soft tissue sarcomas:
- Age:
- Soft tissue sarcomas can occur at any age, but they are most commonly diagnosed in adults. The risk generally increases with age.
- Genetic Factors:
- In some cases, a family history of soft tissue sarcomas or certain genetic syndromes may increase the risk. Examples include Li-Fraumeni syndrome and neurofibromatosis.
- Radiation Exposure:
- Individuals who have undergone previous radiation therapy for cancer treatment, especially during childhood, may have an elevated risk of developing soft tissue sarcomas in the irradiated area.
- Chemical Exposures:
- While rare, exposure to specific chemicals and toxins in the workplace or environment has been linked to an increased risk of soft tissue sarcomas. These exposures may include certain herbicides, dioxins, and chlorophenols.
- Lymphedema:
- Chronic lymphedema, often resulting from lymph node removal during cancer treatment, can slightly increase the risk of developing a specific subtype of soft tissue sarcoma called angiosarcoma.
- Injury or Trauma:
- Some studies suggest that previous injuries or trauma to soft tissues may be associated with a slightly higher risk of developing soft tissue sarcomas. However, this link is not well-established.
- Prior Cancer Treatment:
- Individuals who have received certain chemotherapy agents or radiation therapy as part of their cancer treatment may be at a slightly higher risk of developing soft tissue sarcomas as a secondary cancer.
- Gender:
- Soft tissue sarcomas can affect both males and females. However, some subtypes may have a slight predilection for one gender over the other.
- Race and Ethnicity:
- The risk of soft tissue sarcomas can vary among different racial and ethnic groups, although the reasons for these disparities are not entirely clear.
It’s important to note that while these risk factors may increase the likelihood of developing soft tissue sarcomas, many cases occur in individuals with no known risk factors. Additionally, soft tissue sarcomas are relatively rare, making them less likely to occur than more common cancers. Regular check-ups and early medical evaluation for any concerning symptoms or lumps are crucial for timely diagnosis and treatment.
Diagnosis:
- Imaging: X-rays, CT scans, MRI, and PET scans are used to visualize the tumor’s location, size, and extent.
- Biopsy: A tissue sample (biopsy) is obtained through surgery or needle aspiration to confirm the diagnosis and identify the specific subtype.
- Staging: The cancer is staged to determine its spread and guide treatment decisions.
here are key points about the diagnosis of soft tissue sarcomas:
- Medical History and Physical Examination:
- The diagnostic process typically begins with a thorough medical history review, including any symptoms and risk factors.
- A physical examination is conducted to assess the presence of a lump, mass, or any other concerning signs.
- Imaging Tests:
- X-rays: Initial imaging often involves X-rays to identify the location and size of the tumor.
- CT Scan (Computed Tomography): CT scans provide detailed cross-sectional images of the tumor and surrounding tissues, aiding in diagnosis and staging.
- MRI (Magnetic Resonance Imaging): MRIs offer high-resolution images, particularly useful for evaluating soft tissue tumors’ extent and characteristics.
- PET Scan (Positron Emission Tomography): PET scans can help determine whether the cancer has spread to other areas of the body.
- Biopsy:
- A biopsy is the definitive diagnostic procedure. It involves the removal of a tissue sample from the tumor for laboratory examination.
- Needle Biopsy: In some cases, a fine needle is used to extract a small tissue sample from the tumor.
- Surgical Biopsy: In other cases, a surgical procedure may be required to remove a larger tissue sample.
- Biopsy results confirm the presence of cancer, determine the specific subtype, and guide treatment decisions.
- Staging:
- After diagnosis, staging is crucial to assess the extent of the cancer’s spread. Staging helps determine the most appropriate treatment plan.
- Staging may involve additional imaging tests, such as CT or MRI scans, to evaluate lymph nodes and distant organs for signs of metastasis (spread).
- Genetic Testing:
- Genetic testing may be recommended to identify specific genetic mutations associated with certain soft tissue sarcomas.
- This information can help tailor treatment approaches, including targeted therapies.
- Consultation with a Sarcoma Specialist:
- Due to the rarity and complexity of soft tissue sarcomas, seeking consultation with a sarcoma specialist or a multidisciplinary team is often advisable.
- These experts can provide personalized treatment recommendations based on the tumor’s subtype, location, stage, and individual patient factors.
- Second Opinion:
- Patients diagnosed with soft tissue sarcomas may consider seeking a second opinion to ensure a thorough evaluation and explore various treatment options.
- Monitoring and Follow-Up:
- After diagnosis and initial treatment, patients typically undergo regular follow-up appointments and imaging tests to monitor the tumor’s response to treatment and check for recurrence.
- Clinical Trials:
- Participation in clinical trials may be an option for some patients, providing access to cutting-edge treatments and therapies.
Early and accurate diagnosis of soft tissue sarcomas is essential for developing an effective treatment plan and improving outcomes. Patients are encouraged to work closely with their healthcare providers and seek specialized care to receive the most appropriate and tailored management for their specific diagnosis.
Treatment Options:
Treatment for soft tissue sarcomas typically involves a combination of the following approaches:
- Surgery: The primary treatment is surgical removal of the tumor. In some cases, limb-sparing surgery is possible to preserve function.
- Radiation Therapy: Radiation may be used before or after surgery to target remaining cancer cells and reduce the risk of recurrence.
- Chemotherapy: Chemotherapy may be recommended, particularly for high-grade or advanced sarcomas.
- Targeted Therapy: Some specific subtypes of soft tissue sarcomas respond to targeted therapies that aim to block specific genetic mutations.
- Immunotherapy: Emerging treatments involve harnessing the immune system to fight cancer, but its effectiveness in soft tissue sarcomas is still being studied.
- Clinical Trials: Participation in clinical trials may provide access to innovative treatments and therapies.
Conclusion
Soft tissue sarcomas are a group of rare but diverse cancers that can affect various parts of the body. Early diagnosis, accurate staging, and a tailored treatment plan are crucial for improving outcomes. If you or a loved one experience symptoms or risk factors associated with soft tissue sarcomas, it is essential to consult with a healthcare provider who can guide you through the diagnostic and treatment process. Advances in research and treatment options offer hope for those affected by this condition, emphasizing the importance of early detection and comprehensive care.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023