Urinary Incontinence: Understanding Causes, Symptoms, and Management
Urinary incontinence is a common yet often underestimated condition that affects individuals across various age groups and backgrounds. This involuntary loss of bladder control can significantly impact one’s quality of life, leading to embarrassment, social withdrawal, and a sense of isolation. In this exploration, we delve into the multifaceted aspects of urinary incontinence, shedding light on its causes, recognizing symptoms, and exploring the diverse strategies available for effective management.
Understanding Urinary Incontinence:
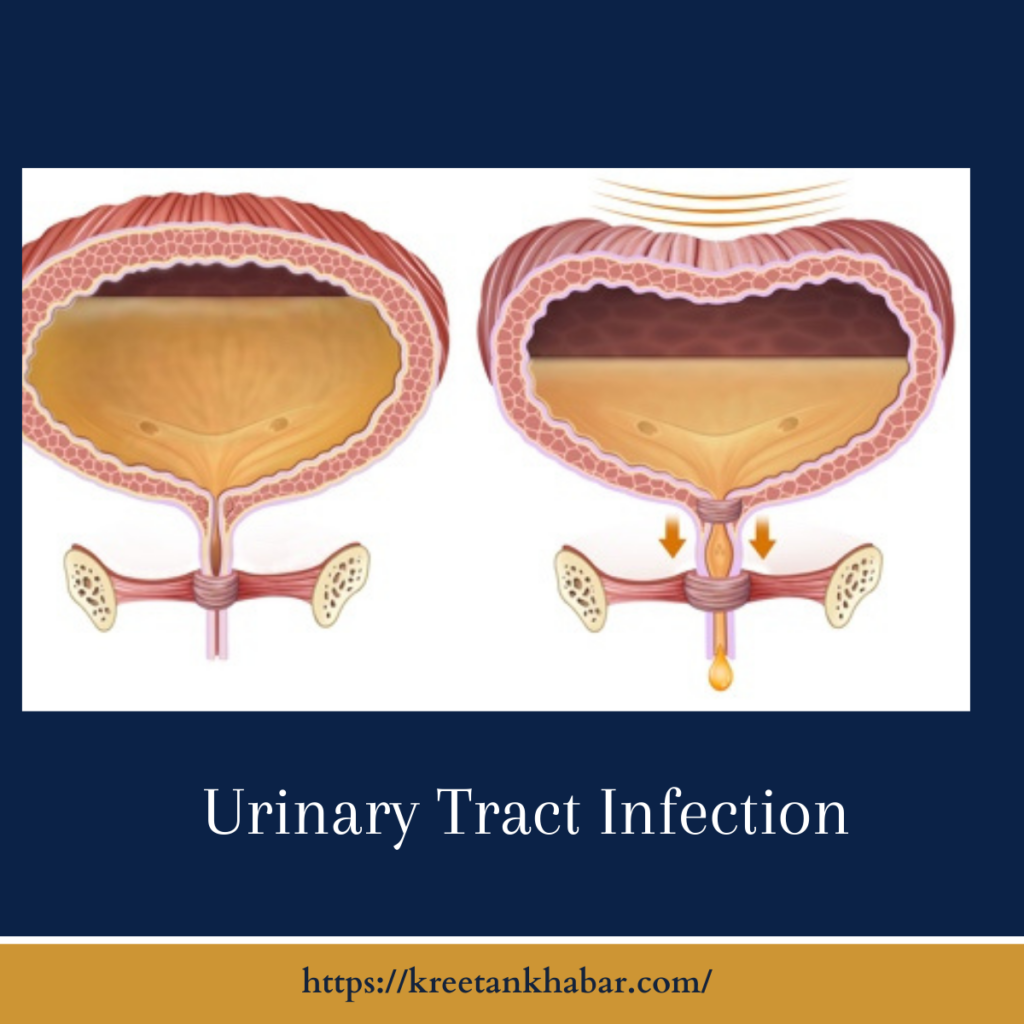
Urinary incontinence is characterized by the unintentional leakage of urine, and it can manifest in different forms. Stress incontinence occurs during activities that exert pressure on the bladder, such as coughing or laughing. Urgency incontinence involves a sudden, intense urge to urinate, often resulting in an inability to reach the toilet in time. Overflow incontinence is characterized by frequent or constant dribbling of urine due to an inability to empty the bladder completely.
Causes of Urinary Incontinence:
- Muscle Weakness: Weakened pelvic floor muscles, often linked to factors like childbirth and aging, can contribute to stress incontinence.
- Nerve Damage: Conditions such as diabetes or neurological disorders can impair the signals between the bladder and the brain, leading to incontinence.
- Hormonal Changes: Menopause and hormonal fluctuations can affect the strength and elasticity of the muscles supporting the bladder.
- Enlarged Prostate: In men, an enlarged prostate can create obstacles to urine flow, leading to overflow incontinence.
- Medications: Certain medications, such as diuretics or those affecting nerve function, may contribute to urinary incontinence.
Symptoms of Urinary Incontinence:
- Involuntary Leakage: The primary symptom is the unintentional release of urine, ranging from a few drops to a complete loss.
- Frequent Urination: Individuals with urgency incontinence may experience a sudden and strong need to urinate more often than usual.
- Nocturia: Waking up frequently during the night to urinate is another common symptom, impacting both sleep quality and overall well-being.
- Hesitation or Straining: Difficulty initiating or completing urination may be observed, particularly in cases of overflow incontinence.
- Involuntary Leakage: The hallmark symptom of urinary incontinence is the unintentional release of urine, varying from small leaks to complete loss of bladder control.
- Stress Incontinence: Activities such as coughing, laughing, sneezing, or exercising can trigger leakage, indicating stress incontinence.
- Urgency: Sudden and intense urges to urinate that are difficult to control, often leading to episodes of urgency incontinence.
- Frequent Urination: Individuals with urinary incontinence may experience an increased frequency of urination, disrupting daily routines and sleep patterns.
- Nocturia: Waking up multiple times during the night to urinate, impacting overall sleep quality and contributing to fatigue.
- Hesitancy or Straining: Difficulty initiating or completing urination, particularly noticed in cases of overflow incontinence.
- Changes in Urination Patterns: Any noticeable alterations in urination patterns, such as a weak stream or difficulty emptying the bladder completely.
- Physical Discomfort: Pelvic pain or discomfort may accompany urinary incontinence, influencing an individual’s overall sense of well-being.
- Emotional Impact: Symptoms of urinary incontinence can evoke feelings of embarrassment, anxiety, or social withdrawal, underscoring the emotional toll of the condition.
- Altered Lifestyle: Individuals with urinary incontinence may modify their lifestyle, such as avoiding certain activities or limiting fluid intake, to cope with the symptoms.
- Impact on Quality of Life: The collective impact of these symptoms can significantly affect an individual’s quality of life, emphasizing the importance of seeking professional guidance for effective management.
Management Strategies:
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles through Kegel exercises can be effective, especially for stress incontinence.
- Behavioral Techniques: Bladder training, scheduled voiding, and fluid management strategies help regulate and improve bladder control.
- Lifestyle Modifications: Dietary adjustments, weight management, and avoiding irritants like caffeine and alcohol can contribute to symptom improvement.
- Medications: Depending on the type of incontinence, medications such as anticholinergics or beta-3 agonists may be prescribed to manage symptoms.
- Pessaries: In some cases, especially with pelvic organ prolapse, the use of pessaries can provide support to the bladder and reduce incontinence.
- Biofeedback and Electrical Stimulation: These therapeutic approaches aim to improve muscle function and coordination for individuals with weakened pelvic floor muscles.
- Surgical Interventions: In certain cases, surgical procedures may be considered, ranging from slings for stress incontinence to more complex reconstructions for structural issues.
Seeking Support and Professional Guidance:
Urinary incontinence is a treatable condition, and seeking support from healthcare professionals is crucial. Open communication, an accurate diagnosis, and a personalized treatment plan tailored to the individual’s specific circumstances contribute to effective management. By fostering awareness and understanding, we can empower individuals affected by urinary incontinence to navigate the challenges and regain control over their bladder health.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023