Uterine Fibroids: Navigating Causes, Symptoms, and Treatment Options
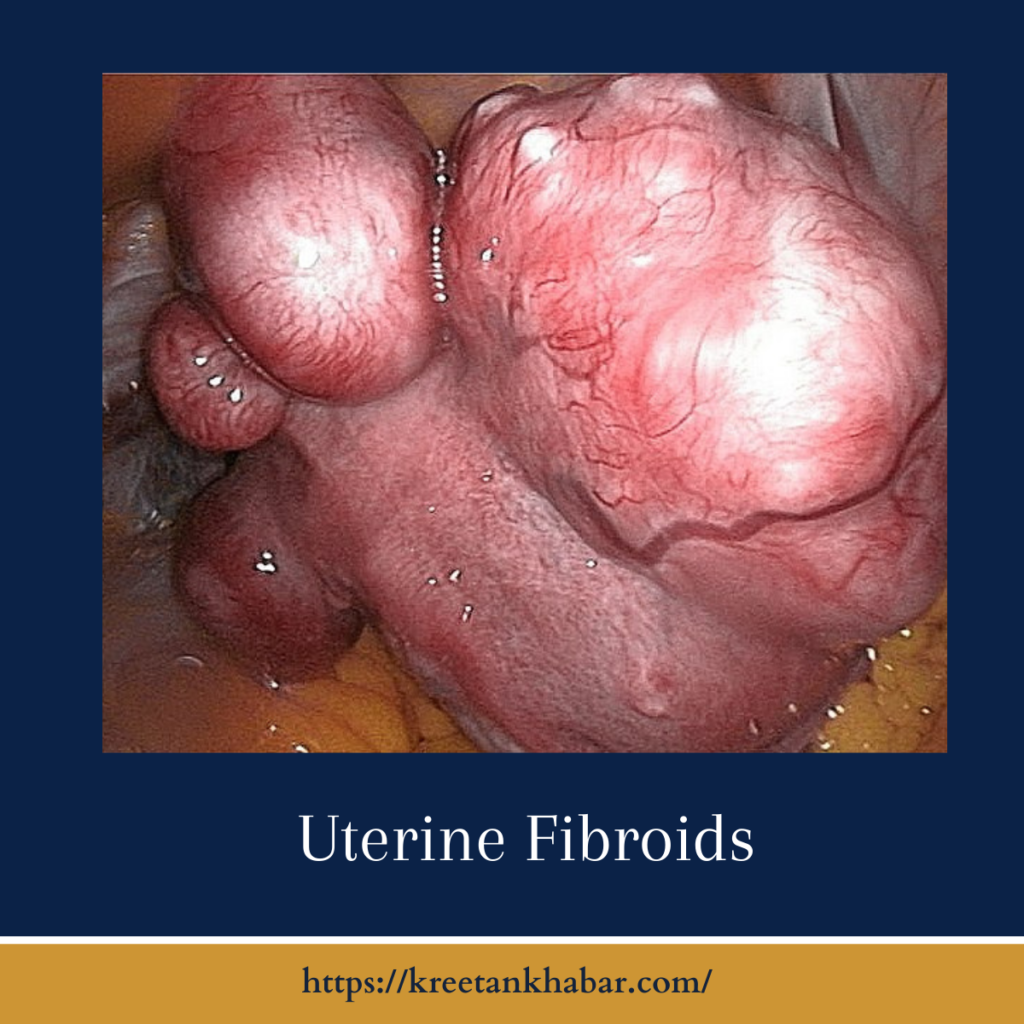
Uterine fibroids, noncancerous growths that develop in the uterus, are a prevalent health concern affecting many women. These benign tumors, also known as myomas or leiomyomas, vary widely in size and can present with an array of symptoms that impact women’s reproductive health. In this exploration, we delve into the complexities of uterine fibroids, shedding light on their causes, recognizing symptoms, and exploring the diverse landscape of treatment options available to address this common gynecological condition.
Causes of Uterine Fibroids:
The exact cause of uterine fibroids remains elusive, but several factors are thought to contribute to their development. Genetic predisposition plays a role, with a family history of fibroids increasing the likelihood of their occurrence. Hormonal influences, particularly estrogen and progesterone, are implicated, as fibroids often grow during reproductive years when hormone levels are at their peak. Additionally, ethnicity, age, and lifestyle factors, such as obesity and diet, may influence the risk of developing fibroids.
Symptoms of Uterine Fibroids:
Uterine fibroids can manifest with a range of symptoms, and their impact can vary from woman to woman. Common indications include:
- Menstrual Irregularities: Fibroids can cause heavy menstrual bleeding, prolonged periods, or irregular menstrual cycles.
- Pelvic Pain and Pressure: Large fibroids or those pressing on surrounding organs may lead to pelvic pain, discomfort, or a feeling of fullness.
- Frequent Urination: Fibroids that press against the bladder can result in increased frequency of urination.
- Constipation: Fibroids affecting the rectum may cause constipation or difficulty with bowel movements.
- Backache or Leg Pains: Pressure on nerves in the back or pelvis may cause backache or leg pains.
- Painful Intercourse: Fibroids can contribute to discomfort or pain during sexual intercourse.
- Enlarged Abdomen: In some cases, a woman with fibroids may notice an enlargement of the lower abdomen.
Diagnosis and Medical Evaluation:
Diagnosing uterine fibroids typically involves a combination of medical history review, pelvic examination, and imaging studies. Ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be utilized to visualize the size, location, and characteristics of the fibroids. Hysteroscopy or laparoscopy, minimally invasive procedures, may be recommended for a more detailed assessment.
Treatment Options:
The management of uterine fibroids depends on factors such as the size and location of the fibroids, the severity of symptoms, and a woman’s reproductive goals. Treatment options include:
- Watchful Waiting: For asymptomatic or mild cases, a watchful waiting approach may be adopted, monitoring the fibroids without active intervention.
- Medications: Hormonal medications, such as birth control pills or GnRH agonists, may be prescribed to regulate menstrual cycles and alleviate symptoms.
- Uterine Fibroid Embolization (UFE): UFE is a minimally invasive procedure that involves blocking the blood vessels supplying the fibroids, leading to their shrinkage.
- Myomectomy: Myomectomy is a surgical procedure to remove individual fibroids while preserving the uterus. It is an option for women who wish to maintain fertility.
- Hysterectomy: In cases where fibroids are severe, and fertility is not a concern, a hysterectomy, the surgical removal of the uterus, may be recommended.
- Endometrial Ablation: This procedure involves the removal or destruction of the uterine lining and is often used to manage heavy menstrual bleeding associated with fibroids.
Living with Uterine Fibroids:
While uterine fibroids can be challenging, many women find effective relief through a combination of medical management and, when necessary, surgical interventions. Open communication with healthcare providers, regular check-ups, and a proactive approach to reproductive health contribute to a more informed and empowered experience for women navigating uterine fibroids.
In conclusion
understanding uterine fibroids empowers women to make informed decisions about their health. By recognizing the causes, symptoms, and available treatment options, women can navigate this aspect of reproductive health with confidence and seek the support needed for optimal well-being.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023