Vibriosis: Unraveling the Intricacies of a Marine Menace
In the vast tapestry of infectious diseases, one that emerges from the depths of marine ecosystems often takes center stage: Vibriosis. This enigmatic condition, caused by various species of the Vibrio bacteria, invites us to delve into the intricate interplay between marine environments, human health, and the nuances of prevention and treatment.
The Ocean’s Microbial Symphony:
Vibriosis finds its origins in the intricate microbial symphony of our oceans. Vibrio bacteria, particularly Vibrio vulnificus and Vibrio parahaemolyticus, thrive in warm coastal waters, showcasing their adaptability to marine ecosystems. While these bacteria play essential roles in marine ecology, their potential to cause illness in humans adds a layer of complexity to our relationship with the ocean.
Sources of Vibriosis:
Encounters with Vibrio bacteria can occur through various channels. Consuming raw or undercooked seafood, especially shellfish like oysters, poses a risk, as does exposure to seawater with open wounds or cuts. The dynamic nature of Vibrio’s habitat means that individuals engaging in marine activities or consuming seafood must be aware of the potential risks.
Clinical Portrait of Vibriosis:
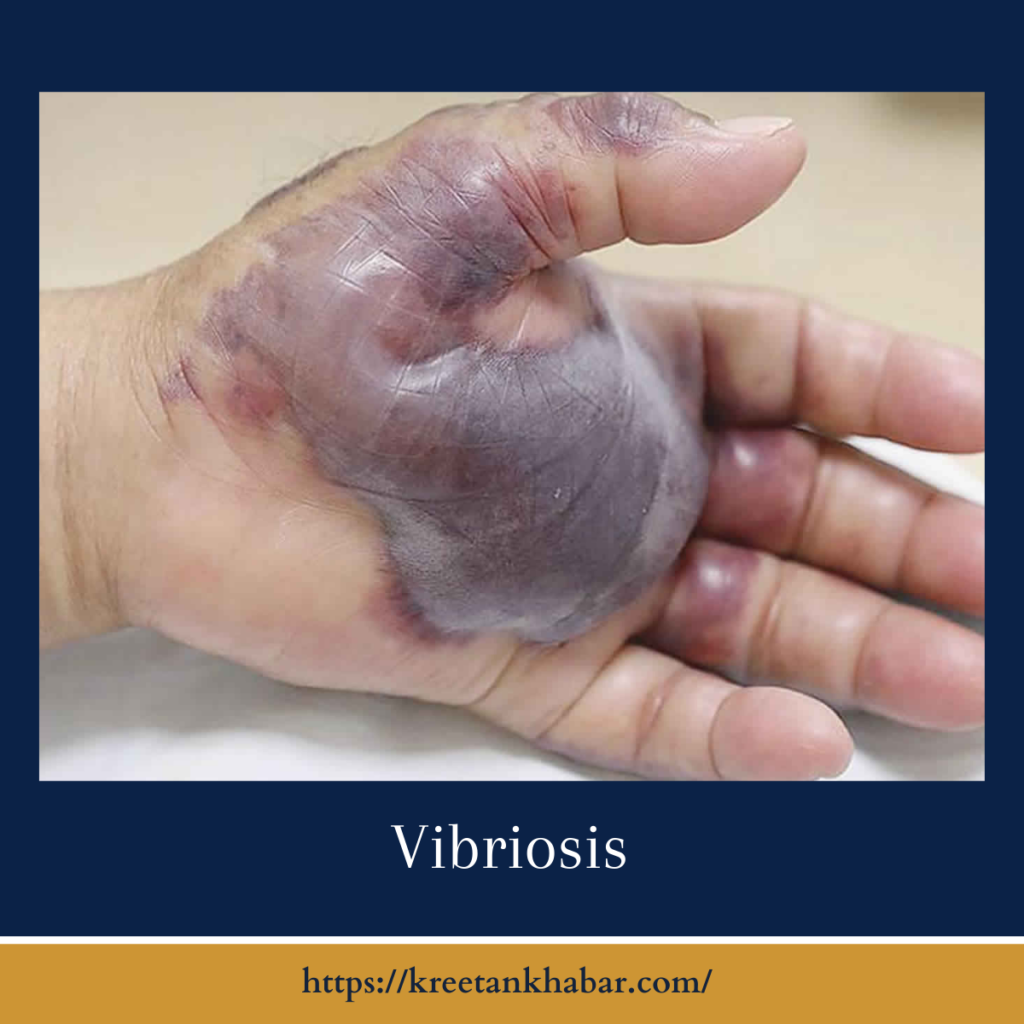
Vibriosis presents a spectrum of clinical manifestations, ranging from mild gastrointestinal discomfort to severe, life-threatening infections. Gastrointestinal symptoms may include nausea, vomiting, abdominal pain, and diarrhea, while more severe cases can lead to bloodstream infections and skin infections when wounds come into contact with contaminated water.
High-Risk Individuals:
Certain individuals face a higher risk of severe vibriosis. Those with compromised immune systems, liver diseases, or underlying health conditions are more susceptible to severe outcomes. Understanding these risk factors is crucial for targeted prevention and early intervention.
Preventive Measures: Navigating the Waters Safely:
Preventing vibriosis involves a combination of awareness and practical measures. Adhering to the following guidelines can significantly reduce the risk of infection:
- Cook Seafood Thoroughly:
- Ensure that seafood, especially shellfish, is cooked thoroughly before consumption. Cooking destroys Vibrio bacteria, minimizing the risk of infection.
- Avoid Raw Seafood with Open Wounds:
- Individuals with open wounds or cuts should avoid exposing them to raw or undercooked seafood and seawater. Vigilance in these situations is paramount.
- Practice Good Hygiene:
- Emphasize good hygiene practices, including handwashing after handling raw seafood and before eating. This simple yet effective measure reduces the risk of Vibrio transmission.
- Choose Seafood Sources Wisely:
- Select reputable sources for seafood. When dining out, choose establishments with a strong track record of food safety to minimize the risk of Vibrio contamination.
- Protect Open Wounds in Seawater:
- If you have open wounds or cuts, take precautions when entering seawater. Using waterproof bandages or protective coverings can prevent direct exposure to Vibrio-containing seawater.
- Be Mindful of High-Risk Activities:
- Individuals with underlying health conditions should exercise caution when engaging in high-risk marine activities. Awareness of personal risk factors can guide decisions about water-related activities.
- Prompt Medical Attention:
- Seek prompt medical attention if symptoms of vibriosis develop, especially for individuals in high-risk groups. Early diagnosis and treatment significantly improve outcomes.
Treatment Landscape:
The treatment of vibriosis varies based on the severity of the infection. Mild cases may not require specific medical intervention and can resolve on their own. However, severe cases, particularly those leading to bloodstream infections, demand immediate medical attention. Antibiotics play a crucial role in managing severe vibriosis and preventing complications.
- Individualized Approach:
- Vibriosis treatment is often tailored to the severity of the infection and the individual’s health status. A personalized approach ensures that the intervention aligns with the specific needs of the patient.
- Mild Cases:
- Mild cases of vibriosis may not necessitate specific medical treatment. The body’s immune system can often manage the infection, and supportive measures such as hydration and rest may be sufficient.
- Antibiotics for Severe Cases:
- Severe cases of vibriosis, especially those leading to bloodstream infections or affecting individuals with compromised immune systems, often require antibiotics. Prompt initiation of antibiotic therapy is crucial to prevent complications.
- Hospitalization in Critical Cases:
- Critical cases of vibriosis, where the infection has progressed to a severe stage, may require hospitalization. This allows for close monitoring, intravenous administration of antibiotics, and supportive care.
- Fluid Replacement:
- Maintaining hydration is a key component of vibriosis treatment. In severe cases with symptoms like vomiting and diarrhea, intravenous fluid replacement may be necessary to prevent dehydration.
- Close Monitoring of Symptoms:
- Continuous monitoring of symptoms is essential throughout the treatment process. This enables healthcare professionals to assess the effectiveness of interventions and make adjustments as needed.
- Prevention of Complications:
- Timely and appropriate treatment aims not only to address the current infection but also to prevent complications. Vigilance in managing severe cases helps minimize the risk of long-term health issues.
- Collaboration Between Healthcare Providers:
- Treatment often involves collaboration between healthcare providers, including primary care physicians, infectious disease specialists, and, if necessary, critical care specialists. This interdisciplinary approach ensures comprehensive care.
- Consideration of Underlying Health Conditions:
- Individuals with underlying health conditions, such as liver diseases or immunocompromised states, may require special attention in treatment planning. Factoring in these conditions enhances the effectiveness of interventions.
- Patient Education:
- Educating patients about the nature of vibriosis, the importance of completing prescribed antibiotic courses, and recognizing signs of complications empowers individuals in their recovery journey.
- Follow-up Care:
- After the acute phase of treatment, follow-up care is essential. This includes monitoring for any lingering symptoms, assessing the resolution of the infection, and addressing any potential long-term effects.
- Adherence to Antibiotic Regimen:
- Adherence to the prescribed antibiotic regimen is critical. Completing the full course of antibiotics, even if symptoms improve before completion, helps prevent the development of antibiotic-resistant strains.
- Adaptive Approaches:
- The treatment landscape may adapt based on emerging strains of Vibrio bacteria and their susceptibility to antibiotics. Staying informed about these dynamics informs healthcare decisions.
- Global Health Considerations:
- In cases involving travel or exposure in different regions, considering global health factors, such as antibiotic resistance patterns, guides treatment choices and ensures a comprehensive approach.
- Psychosocial Support:
- Acknowledging the psychological impact of severe infections, providing psychosocial support is part of holistic care. This may involve addressing anxiety, stress, or any mental health challenges arising from the experience.
Understanding the nuanced treatment landscape of vibriosis involves recognizing the individuality of each case, considering the severity of the infection, and prioritizing collaboration among healthcare professionals. By navigating these points with care, the treatment journey becomes a comprehensive and patient-centered endeavor.
Conclusion:
Navigating the Waters of Awareness:
In navigating the waters of vibriosis, awareness becomes our compass. Understanding the dynamics of Vibrio bacteria, recognizing potential sources of infection, and adopting preventive measures empower individuals to enjoy the bounty of the ocean safely. As we embark on this journey, the synergy between responsible seafood consumption, good hygiene practices, and informed decision-making forms the cornerstone of vibriosis prevention, allowing us to navigate the waters with awareness, respect, and a commitment to public health.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023