Ankylosing Spondylitis: Unraveling the Mystery of a Hidden Disease
Introduction
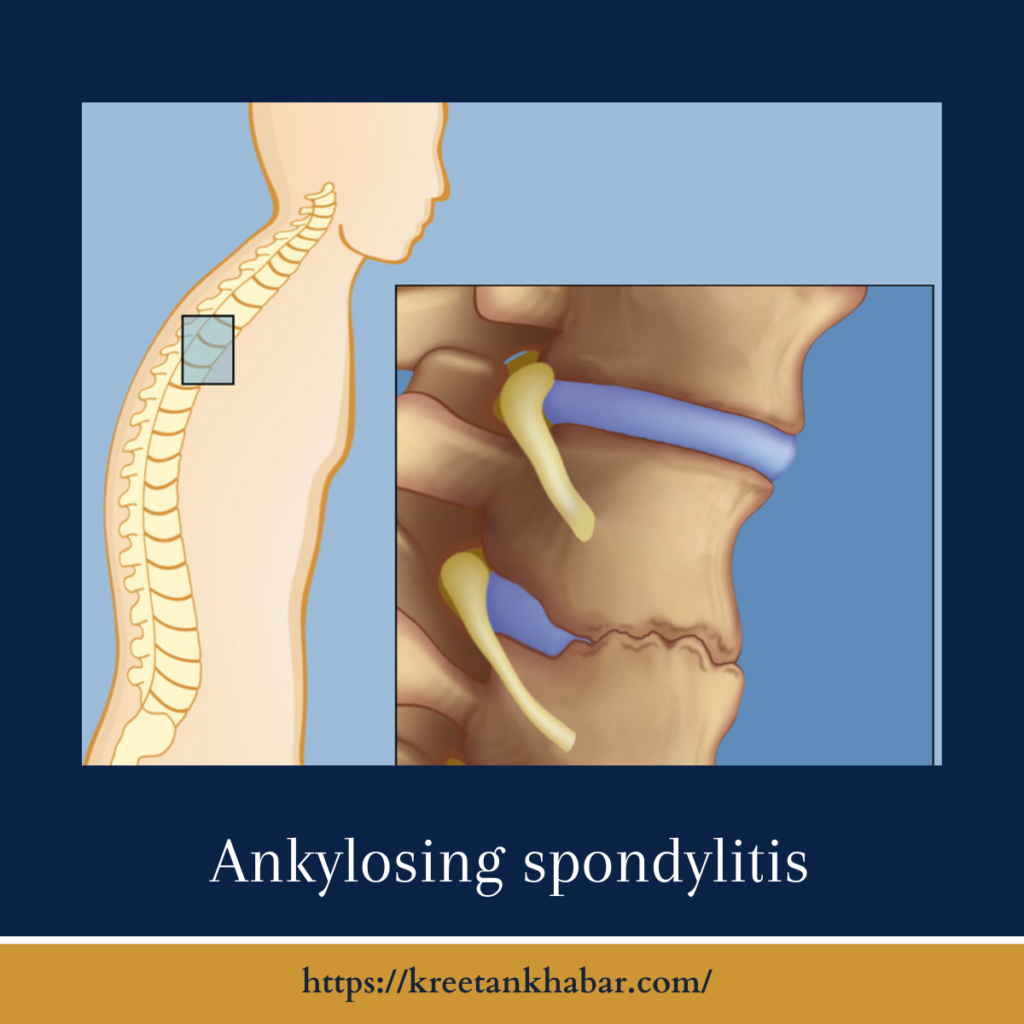
Ankylosing spondylitis (AS) is a complex and relatively lesser-known chronic inflammatory disease that primarily affects the spine and sacroiliac joints. While AS can be challenging to diagnose and manage, understanding its causes, symptoms, and treatment options is crucial for individuals living with this condition. In this article, we will delve into the enigmatic world of ankylosing spondylitis, shedding light on its characteristics and the hope for a better quality of life for those affected.
What Is Ankylosing Spondylitis?
Ankylosing spondylitis is a type of arthritis that predominantly targets the spine. This condition falls under the broader category of spondyloarthritis, which encompasses various inflammatory joint diseases. In AS, chronic inflammation can lead to the fusion of vertebrae, resulting in reduced spinal mobility and a distinctive stooped posture. It typically starts in early adulthood, often affecting men more than women.
Causes of Ankylosing Spondylitis
The exact cause of ankylosing spondylitis remains a subject of ongoing research. However, several factors are believed to contribute to its development:
- Genetic Predisposition: There is a strong genetic component to AS, with specific genetic markers, such as HLA-B27, playing a significant role. Individuals carrying HLA-B27 are at a higher risk of developing the condition.
- Immune System Dysregulation: AS is an autoimmune disease, meaning the immune system mistakenly attacks healthy tissues. This immune system malfunction triggers inflammation in the joints and surrounding tissues.
- Environmental Factors: While genetics play a substantial role, environmental factors, such as infections or other triggers, may also contribute to the onset of AS in genetically susceptible individuals.
Here are 30 unique points outlining the causes of Ankylosing Spondylitis (AS):
- Genetic Predisposition: AS has a strong genetic component, with specific genes, especially HLA-B27, playing a crucial role in its development.
- HLA-B27 Gene: Carrying the HLA-B27 gene significantly increases the risk of developing AS. However, not all individuals with this gene develop the condition.
- Complex Inheritance: AS has a complex inheritance pattern, involving multiple genes and environmental factors.
- Familial Clustering: Family history of AS or related conditions, such as spondyloarthritis, increases the risk of developing the disease.
- Genome-Wide Association Studies (GWAS): GWAS have identified several other genetic markers associated with AS susceptibility.
- Immune System Dysregulation: AS is considered an autoimmune disease, where the immune system mistakenly attacks healthy tissues, particularly in the spine and joints.
- Environmental Factors: Environmental triggers, such as infections or other factors, may contribute to the onset of AS in genetically susceptible individuals.
- Microbial Involvement: Some theories suggest that certain microbial infections or imbalances in the gut microbiome may trigger AS in genetically predisposed individuals.
- Autoimmune Response: It is believed that the immune system’s response to a perceived threat may lead to chronic inflammation in the spine and sacroiliac joints.
- Inflammatory Cascade: The cascade of inflammation in AS may involve the production of pro-inflammatory cytokines and immune cells targeting joint tissues.
- T Cell Activation: AS is associated with the activation of specific T cells in the immune system, contributing to inflammation.
- Autoantibodies: While not a direct cause, autoantibodies related to AS may be detected in some individuals.
- Antigen Presentation: HLA-B27 may play a role in presenting antigens to T cells, triggering an immune response in AS.
- Sexual Dimorphism: AS is more common in men than women, suggesting hormonal and genetic factors may interact.
- Age of Onset: AS typically begins in early adulthood, with symptoms often appearing between the ages of 17 and 45.
- Geographical Variations: The prevalence of AS varies across geographical regions, possibly influenced by genetic and environmental factors.
- Urban-Rural Divide: Some studies have suggested differences in AS prevalence between urban and rural areas, possibly related to lifestyle and environmental factors.
- Occupational Factors: Certain occupational exposures, such as heavy physical labor or activities that strain the spine, may increase the risk of AS.
- Smoking: Smoking has been linked to an increased risk of developing AS and worsening disease progression.
- Altered Gut Microbiota: Changes in the gut microbiota composition may influence the development of AS.
- Nutritional Factors: Diet and nutrient intake may have an impact on the risk and progression of AS.
- Hormonal Influence: Hormones, such as estrogen and testosterone, may play a role in AS susceptibility, explaining gender differences.
- Comorbidities: Individuals with certain comorbid conditions, like psoriasis or inflammatory bowel disease, are at an increased risk of developing AS.
- Ethnic Differences: AS is more prevalent in certain ethnic groups, such as Caucasians and people of Northern European descent.
- Infectious Triggers: Infections, particularly in the gut or urogenital tract, have been proposed as potential triggers for AS.
Symptoms of Ankylosing Spondylitis
The hallmark symptom of ankylosing spondylitis is chronic pain and stiffness in the spine, particularly in the lower back. However, AS can affect various parts of the body, and its symptoms may include:
- Back Pain: Dull, persistent pain in the lower back and buttocks that tends to worsen with inactivity.
- Morning Stiffness: Stiffness and reduced mobility in the morning or after periods of rest.
- Fatigue: Chronic fatigue often accompanies AS, possibly due to the body’s continuous inflammatory response.
- Painful Joints: Inflammation can also affect peripheral joints like hips, knees, and shoulders.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bones, leading to discomfort and swelling.
- Sacroiliac Joint Pain: Pain and stiffness in the sacroiliac joints, where the spine connects to the pelvis.
- Reduced Chest Expansion: In severe cases, AS can limit chest expansion, making it difficult to breathe deeply.
- Eye Inflammation: Some individuals with AS experience eye inflammation, known as uveitis or iritis, which can cause eye pain, redness, and sensitivity to light.
- Gastrointestinal Symptoms: In rare cases, AS can lead to gastrointestinal issues, such as inflammatory bowel disease (IBD).
Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis can be challenging due to its varied and nonspecific symptoms. A definitive diagnosis typically involves a combination of the following:
- Medical History: A detailed medical history, including family history of AS or related conditions, can provide valuable clues.
- Physical Examination: A physical examination may reveal signs such as limited spinal mobility and tender points.
- Imaging Studies: X-rays and magnetic resonance imaging (MRI) are used to visualize changes in the spine and sacroiliac joints characteristic of AS.
- Blood Tests: While there is no specific blood test for AS, certain markers, such as HLA-B27 and inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), may be elevated in some individuals.
- Assessment of Symptoms: Physicians assess the duration, location, and severity of symptoms to determine if they align with AS diagnostic criteria.
- Referral to Rheumatologist: A rheumatologist, a specialist in autoimmune and inflammatory diseases, is often involved in the diagnostic process.
Treatment Options for Ankylosing Spondylitis
While there is no cure for ankylosing spondylitis, various treatment approaches can help manage symptoms and improve quality of life:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first-line treatment to reduce pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) and biologics may be prescribed for more severe cases.
- Physical Therapy: Physical therapy and regular exercise can help maintain flexibility, reduce pain, and improve posture.
- Hot and Cold Therapy: Applying heat or cold to affected areas can provide relief from pain and stiffness.
- Lifestyle Modifications: Ergonomic adjustments, such as using proper posture and supportive furniture, can ease discomfort.
- Surgery: In rare cases of severe joint damage or spinal deformity, surgical intervention may be necessary to restore function.
- Patient Education: Learning about AS and its management is essential for individuals and their families to cope effectively.
Conclusion
Ankylosing spondylitis is a chronic inflammatory disease that can significantly impact an individual’s quality of life. Early diagnosis, appropriate treatment, and a multidisciplinary approach involving healthcare professionals and patients are vital in managing the condition effectively. While AS may present challenges, ongoing research and therapeutic advancements offer hope for improved outcomes and a better understanding of this enigmatic disease.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023