Leishmaniasis: Unveiling the Silent Threat to Global Health
Introduction
Leishmaniasis (also called a kala-azar), a neglected tropical disease caused by protozoa of the Leishmania genus, is a significant global health concern affecting millions of people in various regions. Often overshadowed by more widely recognized diseases, leishmaniasis quietly persists, causing a range of clinical manifestations. In this article, we will delve into the world of leishmaniasis, exploring its causes, types, symptoms, diagnosis, treatment, and the critical need for preventive measures.
The Intricate World of Leishmaniasis
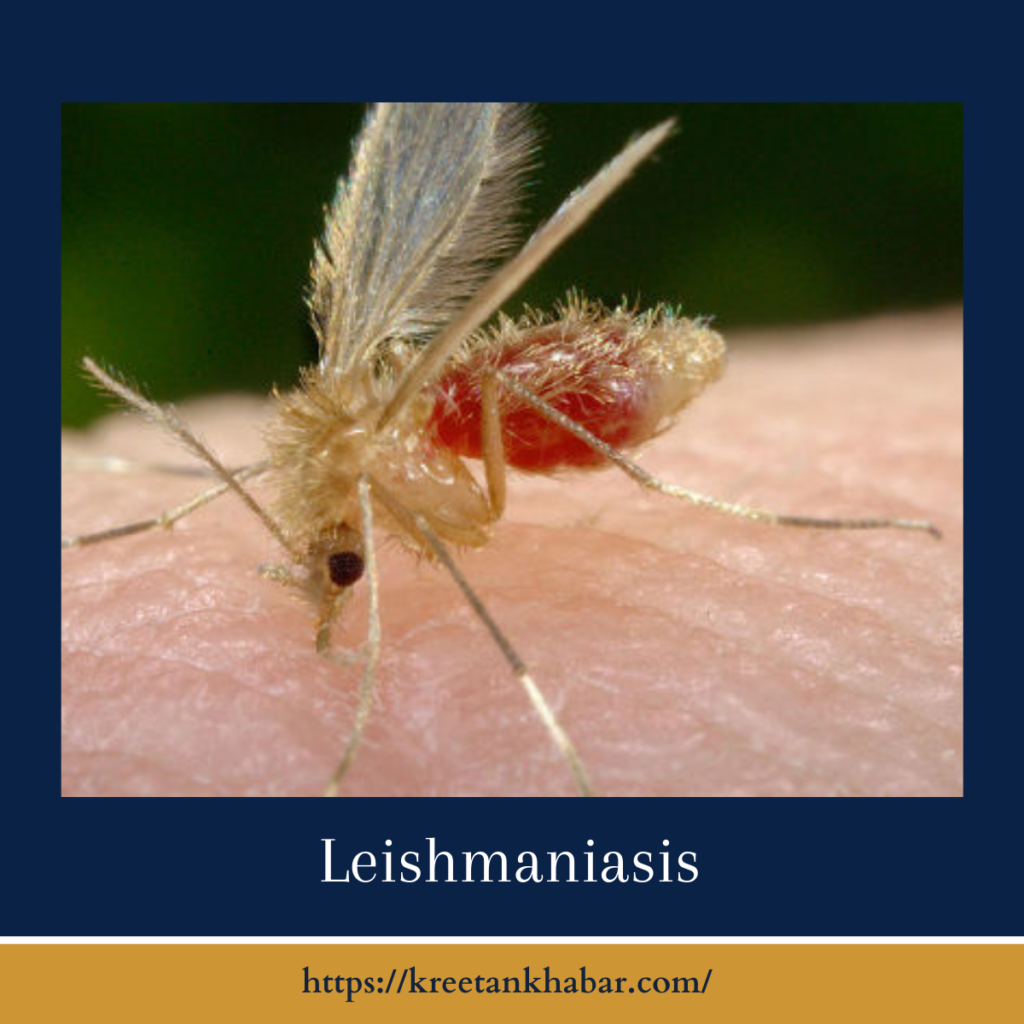
Leishmaniasis is transmitted through the bite of infected female sandflies belonging to the Phlebotomus and Lutzomyia genera. There are three primary forms of leishmaniasis:
- Cutaneous Leishmaniasis: This form affects the skin and is the most common, resulting in ulcerative skin lesions.
- Mucocutaneous Leishmaniasis: This more severe form can disfigure the mucous membranes of the nose, mouth, and throat in addition to the skin.
- Visceral Leishmaniasis: Also known as kala-azar, this form affects internal organs, such as the spleen, liver, and bone marrow, and can be fatal if left untreated.
Causes of Leishmaniasis
Leishmaniasis is caused by protozoa of the Leishmania genus. These parasites have a complex life cycle that involves both sandfly vectors and mammalian hosts, including humans and animals. The disease is prevalent in tropical and subtropical regions, particularly in Africa, Asia, and the Americas.
Here are 30 unique points detailing the causes of leishmaniasis:
- Protozoan Parasites: Leishmaniasis is primarily caused by protozoan parasites of the Leishmania genus.
- Multiple Leishmania Species: Various species of Leishmania can cause different forms of kala-azar, each with varying clinical presentations.
- Complex Life Cycle: The parasites have a complex life cycle involving multiple stages, from the insect vector to the mammalian host.
- Sandfly Vectors: Female sandflies belonging to the Phlebotomus and Lutzomyia genera serve as vectors, transmitting the parasites to humans and animals through their bites.
- Tropical and Subtropical Regions: Leishmaniasis is prevalent in tropical and subtropical regions, where sandflies thrive.
- Zoonotic and Anthroponotic Transmission: Leishmaniasis can be transmitted through zoonotic or anthroponotic cycles, involving animal or human reservoirs, respectively.
- Reservoir Hosts: Various animals, such as rodents, dogs, and wildlife, can act as reservoir hosts for Leishmania parasites.
- Vector-Parasite Interaction: The interaction between sandfly vectors and Leishmania parasites is essential for transmission and infection.
- Environmental Factors: Factors like deforestation, urbanization, and climate change can influence the distribution of sandflies and, consequently, the spread of kala-azar.
- Vector Biting Behavior: Sandflies are typically nocturnal, and their biting behavior during nighttime increases the risk of transmission.
- Human Behavior: Human activities like outdoor work or sleeping outdoors without proper protection can increase the risk of exposure to sandfly bites.
- Host Immunity: Immune responses in infected individuals can influence the severity of the disease and whether it becomes symptomatic or asymptomatic.
- Immunosuppression: Individuals with weakened immune systems, such as those with HIV/AIDS, are more susceptible to severe forms of kala-azar.
- Genetic Factors: Genetic predisposition may play a role in an individual’s susceptibility to kala-azar.
- Malnutrition: Malnourished individuals may be more vulnerable to infection and severe forms of the disease.
- Population Density: Overcrowded living conditions can facilitate the transmission of kala-azar in endemic areas.
- Lack of Access to Healthcare: Limited access to healthcare services can result in delayed diagnosis and treatment, allowing the disease to progress.
- Travel and Migration: People traveling from non-endemic to endemic regions can unknowingly introduce the disease to new areas.
- War and Conflict: Displacement of populations and disrupted healthcare systems in conflict zones can exacerbate the spread of kala-azar.
- Public Health Interventions: The effectiveness of vector control programs and public health initiatives can influence the prevalence of kala-azar.
- Drug Resistance: The emergence of drug-resistant Leishmania strains can complicate treatment and contribute to the persistence of the disease.
- Insecticide Resistance: Sandfly populations can develop resistance to insecticides, reducing the effectiveness of vector control measures.
- Socioeconomic Factors: Poverty and limited access to education can contribute to the spread of kala-azar in vulnerable communities.
- Environmental Changes: Deforestation and changes in land use can alter the habitats of sandfly vectors and affect disease transmission.
- Disease Surveillance: Effective surveillance systems are crucial for monitoring and responding to kala-azar outbreaks.
- Lack of Vaccination: Unlike some other diseases, there is currently no widely available vaccine for kala-azar.
- Behavioral Practices: Cultural practices, such as sleeping outdoors or using traditional medicines, can influence exposure to sandfly bites.
- Peri-urbanization: Expansion of human settlements into previously forested areas can bring people into closer contact with sandfly habitats.
- Globalization: Increased travel and trade can contribute to the spread of kala-azar between regions.
- One Health Approach: A holistic “One Health” approach that considers human, animal, and environmental factors is essential for effective kala-azar control and prevention.
Understanding the multifaceted causes of kala-azar is essential for designing comprehensive strategies to combat this neglected tropical disease and reduce its impact on affected communities.
Symptoms and Clinical Presentation
The symptoms of leishmaniasis vary depending on the form of the disease but may include:
- Cutaneous Leishmaniasis: Skin lesions that can be painless or ulcerate, often resembling boils or ulcers.
- Mucocutaneous Leishmaniasis: Progressive destruction of mucous membranes, leading to facial disfigurement and difficulty in breathing or swallowing.
- Visceral Leishmaniasis: Symptoms may include fever, weight loss, enlargement of the spleen and liver, anemia, and a compromised immune system.
Diagnosis and Treatment
Diagnosing leishmaniasis involves various methods, including:
- Microscopic Examination: Microscopic examination of tissue samples or smears can reveal the presence of Leishmania parasites.
- Serological Tests: Blood tests can detect antibodies to Leishmania, aiding in diagnosis.
- Molecular Tests: Polymerase chain reaction (PCR) assays can identify the parasite’s DNA in samples.
Treatment options for kala-azar typically involve the use of antiparasitic drugs, such as pentavalent antimonials, amphotericin B, or miltefosine. The choice of treatment depends on the type of kala-azar, the region, and drug availability.
Preventing Leishmaniasis
Preventing kala-azar requires a combination of vector control, personal protective measures, and community awareness:
- Vector Control: Controlling sandfly populations through insecticide spraying and environmental management can reduce transmission.
- Protective Clothing: Wearing long sleeves, pants, and insect repellent can prevent sandfly bites.
- Bed Nets: Sleeping under insecticide-treated bed nets can protect against night-biting sandflies.
- Reservoir Control: Identifying and treating infected animals, which can act as reservoirs for the parasite, can reduce transmission.
- Early Diagnosis and Treatment: Early diagnosis and prompt treatment of cases can prevent the progression of the disease and further transmission.
- Community Education: Raising awareness about leishmaniasis, its transmission, and preventive measures is crucial in endemic areas.
Conclusion
Leishmaniasis may remain hidden from the global spotlight, but its impact on millions of lives cannot be ignored. Through enhanced research, early diagnosis, effective treatment, and a concerted effort to prevent transmission, we can work towards reducing the burden of this silent but formidable threat to global health.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023