Osteomyelitis: A Silent Battle within the Bones
Introduction:
Beneath the surface of our skeletal fortress lies a silent battle that often goes unnoticed until it reaches a critical point – osteomyelitis. This formidable condition, characterized by inflammation of the bone and marrow, poses a complex challenge to both patients and healthcare professionals. In this exploration, we delve into the depths of osteomyelitis, unraveling its intricacies and shedding light on the various facets of this often underestimated ailment.
Understanding Osteomyelitis:
Osteomyelitis, derived from the Greek words “osteon” (bone) and “myelo” (marrow), is an infection that infiltrates the bone and its marrow components. While it can affect any bone in the body, it commonly strikes the long bones of the arms and legs, as well as the spine and pelvis. Staphylococcus aureus bacteria are frequently the culprits behind this condition, although other microorganisms can also be responsible.
The Origins of the Battle:
Osteomyelitis can arise from various sources, making it a multifaceted adversary. The most common pathways involve a direct entry of bacteria into the bone, often through an open wound, fracture, or surgery. Hematogenous spread, where bacteria travel through the bloodstream and settle in the bones, is another prevalent route. Additionally, chronic conditions like diabetes or compromised immune systems can heighten the risk of developing osteomyelitis.
Symptoms and Diagnostic Challenges:
Unraveling the mystery of osteomyelitis can be challenging due to its elusive nature. Symptoms may include persistent pain, swelling, warmth, and redness around the affected area, often accompanied by fever and chills. However, these signs can mimic other conditions, leading to diagnostic dilemmas. Advanced imaging techniques, such as MRI and bone scans, are crucial in unraveling the hidden layers of osteomyelitis and confirming its presence.
- Pervasive Pain: Osteomyelitis often announces its presence through persistent, deep-seated pain in the affected bone. The pain may start subtly but tends to intensify over time, creating a constant discomfort that sets it apart from typical aches.
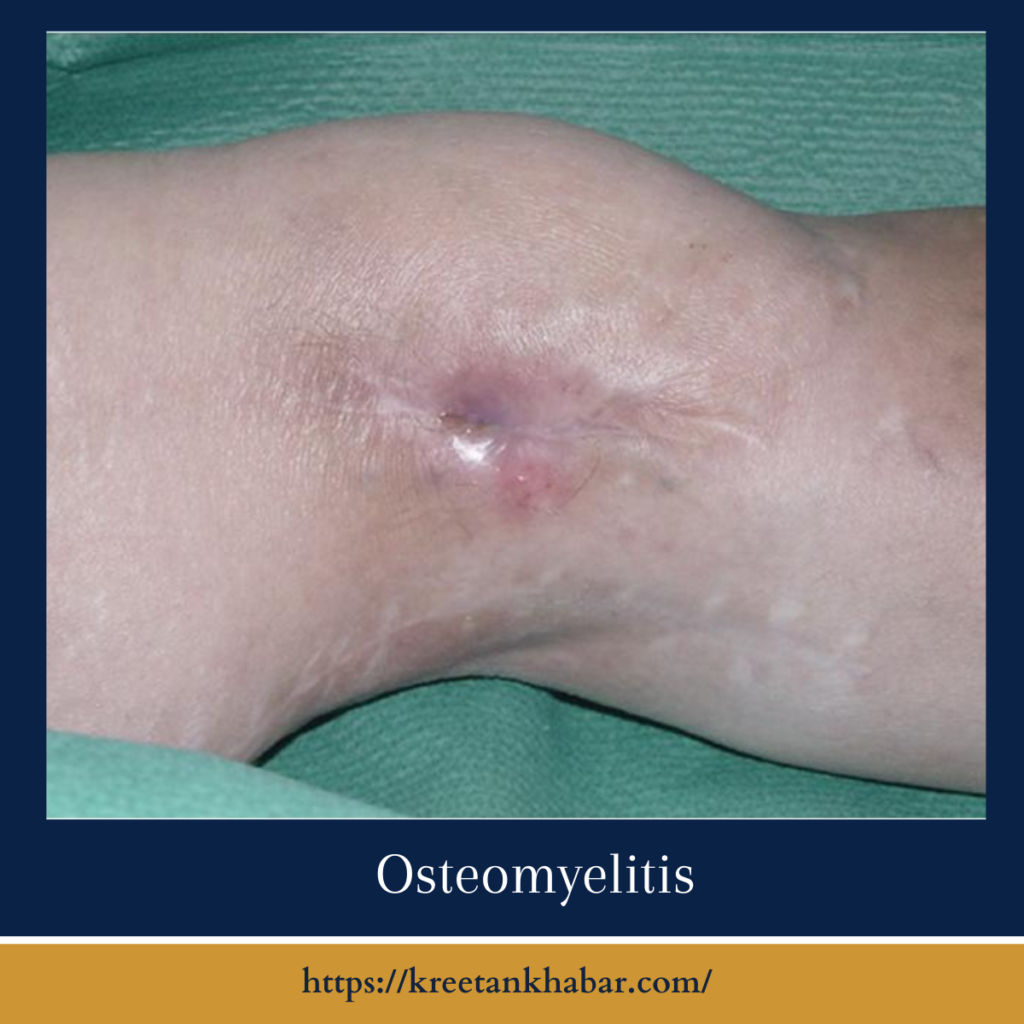
- Localized Swelling and Redness: A visual clue to the ongoing battle within is the swelling and redness that manifests around the infected area. This outward sign indicates the body’s attempt to marshal its defenses against the invading pathogens.
- Unwelcome Heat: Infected bones become hot to the touch as part of the inflammatory response. The warmth emanating from the affected site is a tactile symptom that underscores the ongoing war between the immune system and the invading bacteria.
- Systemic Distress – Fever and Chills: Osteomyelitis is not confined to the battleground; its effects extend systemically. The body reacts to the infection with a rise in temperature, leading to fever and chills as the immune system mobilizes its forces to contain the threat.
- Limited Range of Motion: As the infection progresses, the bone’s ability to function normally is compromised. This can result in a reduced range of motion in nearby joints, a clear indication that the battle is impacting the structural integrity of the bone.
- Generalized Fatigue: The body’s energy reserves are diverted to combat the infection, often leaving individuals with a sense of fatigue and lethargy. This systemic symptom is a subtle yet important indicator of the toll osteomyelitis takes on the overall health of the affected person.
- Visible Wound Issues: If osteomyelitis is a result of an open wound or surgery, the wound may exhibit delayed healing, persistent drainage, or the formation of pus. These issues at the site of entry can be early warning signs of bone involvement.
- Loss of Appetite and Weight Loss: The body’s metabolic response to infection includes a decrease in appetite and subsequent weight loss. Individuals with osteomyelitis may experience a notable decline in their eating habits, contributing to the overall toll on their well-being.
- Mood Swings and Irritability: Dealing with chronic pain and a systemic infection can take a toll on one’s mental health. Mood swings, irritability, and a general sense of unease may accompany the physical symptoms, emphasizing the holistic impact of osteomyelitis.
- Diagnostic Challenges: It’s crucial to note that these symptoms may not always point directly to osteomyelitis. Given the condition’s complexity and the potential overlap with other ailments, accurate diagnosis often requires a combination of clinical evaluation, imaging studies, and laboratory tests.
Recognizing these symptoms and seeking prompt medical attention is vital in the early detection and effective management of osteomyelitis, preventing potential complications and long-term consequences.
Treatment Strategies:
Once the battlefront is identified, the treatment journey begins. Osteomyelitis necessitates a multifaceted approach, often combining antibiotics, surgical intervention, and supportive care. Intravenous antibiotics are typically administered to combat the infection, and surgical procedures may be required to remove infected bone or drainage of abscesses. In severe cases, joint replacements or bone grafts may be necessary to restore functionality.
- Antibiotic Arsenal: The primary weapon in the medical arsenal against osteomyelitis is a course of targeted antibiotics. Intravenous administration is often necessary to ensure the potent drugs reach the site of infection effectively, combating the invading bacteria.
- Surgical Strikes: In severe cases, surgical intervention becomes a critical component of the treatment strategy. Surgeons may need to remove infected bone tissue, drain abscesses, or address any structural damage caused by the infection. This ensures a thorough removal of the bacterial threat.
- Supportive Care: The body’s own defenses play a crucial role in the battle against osteomyelitis. Supportive care measures, including pain management, adequate nutrition, and overall well-being support, enhance the immune system’s ability to wage war against the infection.
- Long-Term Antibiotic Therapy: Osteomyelitis is a resilient foe, often requiring a prolonged course of antibiotics even after the initial acute phase. This long-term therapy aims to prevent a resurgence of the infection and consolidate the gains made during the intensive treatment phase.
- Biofilm Disruption Tactics: Bacterial biofilms, protective layers formed by the microbes, can complicate the treatment process. Novel therapies are emerging to disrupt these biofilms, making the bacteria more vulnerable to antibiotic attack and improving the overall efficacy of treatment.
- Hyperbaric Oxygen Therapy (HBOT): In some cases, hyperbaric oxygen therapy may be employed as an adjunctive treatment. This involves breathing pure oxygen in a pressurized room, creating an environment that enhances the body’s natural healing processes and supports antibiotic effectiveness.
- Bone Grafts and Joint Reconstruction: Extensive bone damage may require additional measures such as bone grafts or joint reconstruction. These procedures aim to restore structural integrity and functionality to the affected bones and joints, facilitating a return to normal activities.
- Patient Education and Compliance: Winning the battle against osteomyelitis also requires active participation from the patient. Understanding the importance of adhering to the prescribed treatment plan, attending follow-up appointments, and maintaining overall health is crucial in preventing recurrence.
- Monitoring for Complications: Osteomyelitis can give rise to complications such as septicemia or the spread of infection to adjacent tissues. Vigilant monitoring for such complications ensures early intervention, preventing the escalation of the battle into more dangerous territory.
- Collaborative Approach: Addressing osteomyelitis is a collaborative effort. A multidisciplinary team, including infectious disease specialists, orthopedic surgeons, nurses, and physical therapists, work in tandem to formulate and execute a comprehensive treatment plan tailored to the individual patient’s needs.
The treatment of osteomyelitis is a dynamic process that combines medical expertise, technological advancements, and the resilience of the human body. This multi-pronged approach aims not only to eradicate the immediate threat but also to pave the way for recovery, ensuring the affected individual can reclaim their quality of life.
The Lingering Impact:
Beyond the immediate skirmish, osteomyelitis can leave a lasting impact on the affected individual. Chronic pain, deformities, and compromised limb function are potential aftermaths, emphasizing the importance of early detection and intervention. Long-term follow-up care becomes paramount to address ongoing challenges and prevent recurrence.
Preventive Measures and Hope on the Horizon:
As with any battle, prevention is a crucial aspect of managing osteomyelitis. Vigilance in wound care, especially for those with diabetes or weakened immune systems, can significantly reduce the risk of infection. Ongoing research endeavors are exploring innovative therapies, including biofilm-disrupting agents and advanced diagnostic tools, offering hope for more effective and targeted interventions in the future.
Conclusion:
In the intricate realm of osteomyelitis, understanding the nuances of its origin, diagnosis, and treatment is essential in navigating the complexities of this bone-deep infection. By unraveling its mysteries, healthcare professionals and patients alike can engage in a collective effort to mitigate its impact and forge a path towards healing and restoration. Osteomyelitis may be a silent battle within the bones, but with knowledge, early intervention, and ongoing research, we can empower ourselves to face it head-on and emerge victorious.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023