Rectocele and Embracing Empowered Solutions
Introduction:
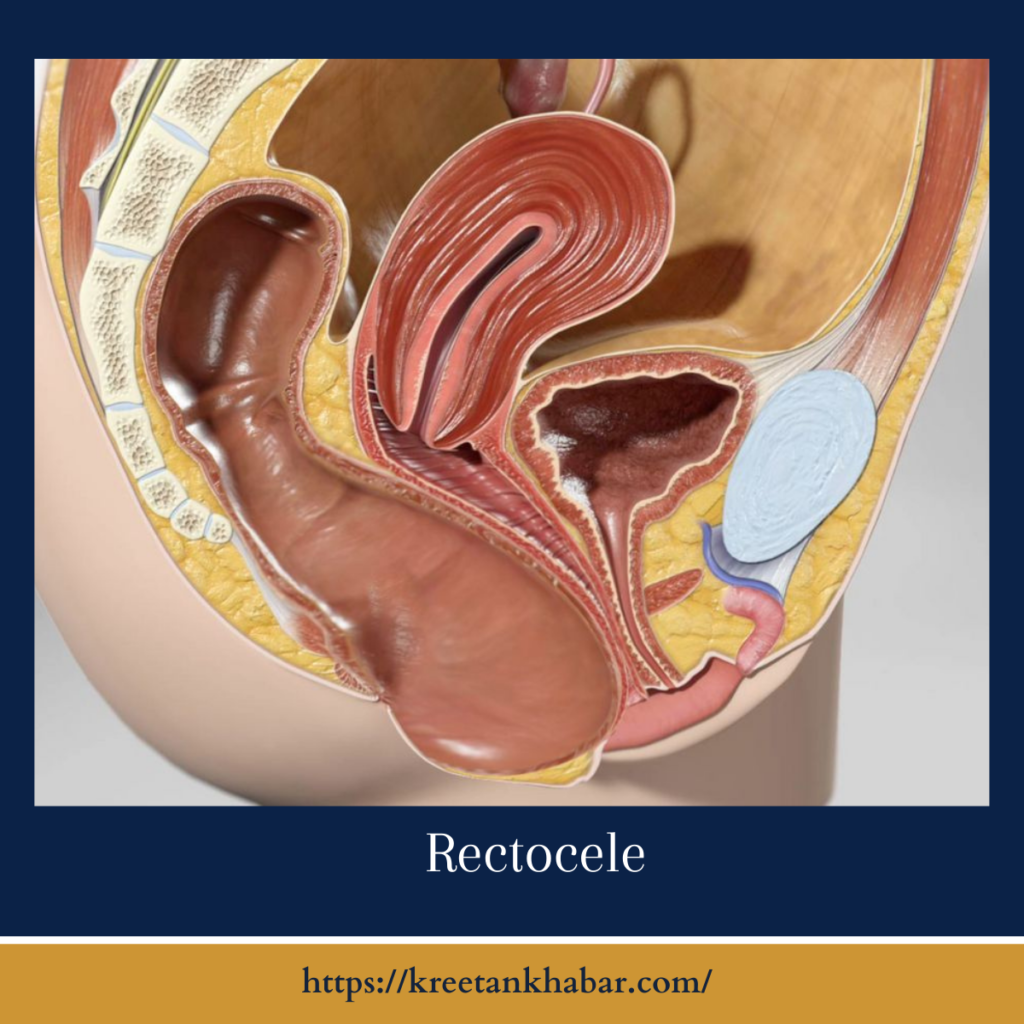
In the tapestry of women’s health, certain concerns often dwell in the shadows, whispered about but rarely openly discussed. Rectocele(also knowna as colpocele), a condition that affects the pelvic floor and can impact a woman’s quality of life, is one such topic. In this exploration, we’ll shine a light on rectocele, unraveling its intricacies, symptoms, and the spectrum of empowered solutions available to those seeking relief.
Decoding Rectocele:
Rectocele is a condition where the thin wall of tissue separating the rectum from the vagina weakens, allowing the rectum to bulge into the vaginal space. While it might not be a dinner table conversation, understanding colpocele is pivotal for women’s health, as it can significantly affect daily life and well-being.
The Unseen Culprits:
Several factors contribute to the development of colpocele, with childbirth being a primary culprit. The strain on the pelvic floor muscles during vaginal deliveries, especially multiple ones, can weaken the supportive tissues. Aging, hormonal changes, chronic constipation, and repeated heavy lifting also play significant roles in the progression of rectocele.
Signs and Symptoms:
Rectocele announces its presence through a set of distinctive signs and symptoms. Women may experience a bulging sensation in the vagina, particularly during bowel movements. Difficulty passing stool, a feeling of incomplete evacuation, and discomfort or pain during sexual intercourse are common indicators. These signals, while sensitive, should not be dismissed but rather addressed with the support of healthcare professionals.
- Bulging Sensation in the Vagina: A notable sign of colpocele is a sensation of bulging or fullness in the vagina. Women may perceive a protrusion, especially during activities like bowel movements or when bearing down.
- Difficulty Passing Stool: colpocele can lead to challenges during bowel movements. Women may experience difficulty in fully evacuating the bowels, often requiring additional effort to pass stool.
- Feeling of Incomplete Evacuation: The persistent feeling of incomplete bowel evacuation is a common symptom. Despite efforts to empty the bowels, individuals with rectocele may sense that not all stool has been expelled.
- Discomfort or Pain During Bowel Movements: Discomfort or pain during bowel movements is another indicator of colpocele. The strain on weakened pelvic floor muscles during defecation can lead to discomfort, ranging from mild to more pronounced pain.
- Pelvic Pressure or Heaviness: Women with colpocele may experience a continuous sense of pelvic pressure or heaviness, particularly after standing for extended periods or engaging in activities that strain the pelvic floor.
- Backache or Lower Abdominal Discomfort: colpocele can contribute to backache or discomfort in the lower abdomen. The strain on pelvic muscles may radiate to the back, creating a persistent ache or discomfort.
- Pain or Discomfort During Sexual Intercourse: For some women, colpocele can lead to pain or discomfort during sexual intercourse. The altered anatomy and pressure on the vaginal wall may contribute to this symptom.
- Visible Bulge in the Vaginal Opening: In more advanced cases, a visible bulge or protrusion may be noticeable at the vaginal opening. This physical manifestation is often more apparent during activities that increase abdominal pressure, like straining during bowel movements.
- Worsening of Symptoms When Standing or Straining: Symptoms of colpocele may intensify when standing for prolonged periods or during activities that involve straining, such as heavy lifting. The increased pressure on the weakened pelvic floor can exacerbate the condition.
- Impact on Quality of Life: Beyond physical symptoms, rectocele can impact overall quality of life. Women may experience emotional distress, embarrassment, or a sense of limitation in daily activities, emphasizing the need for timely intervention and support.
Recognizing these signs and symptoms is crucial for seeking timely medical attention. Early intervention can lead to effective management and an improved quality of life for individuals dealing with rectocele. If any of these symptoms are persistent or causing distress, consultation with a healthcare professional is recommended.
Impact on Quality of Life:
Beyond the physical manifestations, rectocele can have a profound impact on emotional and psychological well-being. Women may grapple with feelings of embarrassment, self-consciousness, or a perceived loss of femininity. It’s crucial to recognize that rectocele is a common and treatable condition, and seeking support is a vital step toward reclaiming a sense of empowerment.
Empowered Solutions:
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles through targeted exercises, such as Kegels, forms the bedrock of non-invasive solutions for rectocele. These exercises enhance muscle tone and provide better support to the pelvic organs.
- Lifestyle Modifications: Adopting lifestyle changes can significantly impact rectocele. Maintaining a healthy weight, addressing chronic constipation through dietary measures, and avoiding heavy lifting contribute to overall pelvic health.
- Pessary Use: Pessaries, supportive devices inserted into the vagina, can provide additional structural support and alleviate symptoms of rectocele. This non-surgical option is particularly beneficial for women who wish to avoid or delay surgery.
- Physical Therapy: Specialized physical therapy focusing on pelvic floor rehabilitation is a hands-on approach to address muscle weaknesses contributing to rectocele. Physical therapists guide individuals through exercises and techniques to improve pelvic floor function.
- Hormone Replacement Therapy (HRT): For women experiencing rectocele due to hormonal changes associated with menopause, hormone replacement therapy may be considered. HRT can help restore estrogen levels, improving the elasticity of pelvic tissues and potentially alleviating symptoms.
- Surgical Interventions: In cases where conservative measures prove insufficient, surgical options, including posterior colporrhaphy, may be considered. These procedures involve repairing and reinforcing the weakened tissues to restore the anatomical support of the vaginal wall.
Embracing Open Dialogue:
Breaking the silence surrounding rectocele is an essential step toward empowerment. Open dialogue between healthcare providers and patients fosters an environment where women feel comfortable discussing their symptoms, seeking guidance, and exploring treatment options. This shared understanding is a cornerstone for effective care.
Conclusion:
Rectocele, while often existing in the realm of unspoken concerns, deserves attention and compassionate care. By shedding light on its intricacies, understanding its impact, and exploring a spectrum of empowered solutions, women can navigate rectocele with resilience and embrace a journey towards holistic well-being. Through open dialogue, support, and comprehensive care, rectocele can be addressed, allowing women to reclaim control over their health and lives.
Read also : Exploring the Delightful Boost of the Green Tea Shot 2023